A parathyroid carcinoma within a cold thyroid nodule
LL Travaini, G Trifiro and G Paganelli
Nuclear Medicine Division, European Institute of Oncology, Via Ripamonti 435, 20141 Milan, Italy
Correspondence to G Paganelli. Email: divisione.medicinanucleare@ieo.it
Abstract
We report the case of a 71-year-old woman who was referred to our institute with a solid nodule in the right thyroid lobe and hypercalcemia. Ultrasound revealed a well-vascularized right thyroid nodule that was identified as a cold area by 99mTc-sodium pertechnetate scan. Fine-needle aspiration showed a follicular lesion and blood tests revealed hypercalcemia and hyperparathyroidism. A 99mTc-methoxyisobutylisonitrile (99mTc-Sestamibi) scan was subsequently performed revealing a focal area of increased uptake in the right thyroid lobe, within the cold area detected by the thyroid scan. A right emithyroidectomy and right superior and inferior parathyroidectomy was performed and histopathological examination showed a parathyroid carcinoma (immunohistochemistry positive for PTH and chromogranin A, Ki-67 10%) associated with follicular hyperplasia.
A 71-year-old woman was referred to our institute with a solid nodule in the right thyroid lobe combined with hyperparathyroidism and hypercalcemia. She had a prior history of infiltrating ductal carcinoma (pT1c pN0) for which she had a right quadrantectomy and axillary lymph node dissection.
Ultrasound (US) revealed a 3.5 ´ 2.7 ´ 2.5 cm well-vascularized nodule in the right thyroid lobe, characterized by cystic and solid components. Fine-needle aspiration indicated a follicular lesion.
A 99mTc-sodium pertechnetate scan showed a large cold area in the right thyroid lobe (Figure 1A).
Blood examination revealed a calcium level of 14.5 mg/dl (normal range 8.1–10.4), a phosphate level of 2.1 mg/dl (normal range 2.7–4.5), a parathyroid hormone (PTH) level of 4480 pg/ml (normal range 14.0–72.0) and normal levels of TSH and thyroglobulin.
A 99mTc-methoxyisobutylisonitrile (99mTc-Sestamibi) scan subsequently performed revealed a focal area of increased uptake in the right thyroid lobe, within the cold area detected by the thyroid scan (Figure 1B and C) and is clearly evident in the subtraction image (Figure 1D). This area of increased uptake indicated tissue with high-mitochondrial activity probably of parathyroid origin.
A right hemithyroidectomy and right superior and inferior parathyroidectomy was performed. Histopathological examination showed a parathyroid carcinoma (immunohistochemically positive for PTH and chromogranin A, Ki-67 10%) associated with follicular hyperplasia.
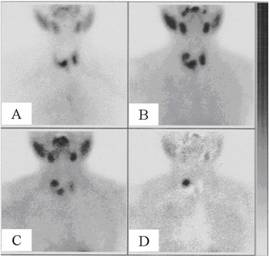
Figure 1: (A) [99mTc] sodium pertechnetate scan shows a cold area in the upper right thyroid lobe. Early (B) and delayed (C) [99mTc] Sestamibi scans reveal a focal area of increased uptake in the upper right thyroid lobe, within the cold area detected by the thyroid [99mTc] sodium pertechnetate scan. (D) Processed image obtained by data subtraction of the [99mTc] Sestamibi scan from the [99mTc] sodium pertechnetate scan.
Discussion
Primary hyperparathyroidism (hPTH) is a disorder that is usually treated by surgery.
In the past, the standard was bilateral neck exploration, but, recently, there has been rapidly developing interest in less invasive surgical management because of the evolution of certain imaging techniques [1–5], which allow precise, preoperative localization of the lesion. 99mTc-Sestamibi, which was initially introduced for cardiac scintigraphy, was accidentally found to accumulate in parathyroid adenomas [6]. The exact mechanism of its elective uptake in abnormal parathyroid glands remains debatable. High-mitochondrial activity is considered to be the major component of Sestamibi uptake by human parathyroid tissue in patients with pHPT [7,8].
This functional imaging has very high specificity for parathyroid tissue, with only a small number of reports of false-positive uptake into lymph nodes or thyroid nodules [9,10].
High-frequency ultrasonography imaging is a highly sensitive technique [11] in experienced hands, but in patients with thyroid nodules, it is less precise [12–14] and is often unable to differentiate between benign and malignant thyroid nodules.
Although there are only a few reports [15,16], which have addressed the diagnostic importance of US for thyroid disease associated with an increase of hPTH, Mihai et al [17] suggest that in cases of hPTH the combined use of 99mTc-Sestamibi and US are two complementary investigating tools.
However, no clear consensus has been reached regarding which protocol to use in such cases.
Reports of concomitant thyroid disease in patients with hPTH date to the early 1950s, with a prevalence ranging from 22% to 70% [16,18,19]. The cause of this association remains controversial: some authors described it as incidental [20], meanwhile others suggest the presence of goitrogenic factors, such as increased endogenous calcium, epithelial growth factor or moreover insulin-like growth factor [19,21,22], may influence the development of thyroid disease. Recently, Masatsugu et al [23] reported that thyroid disease (including non-medullary thyroid carcinoma) occurs frequently in the presence of sporadic hPTH and underlined the importance of pre-operative US for evaluating possible concomitant thyroid disease, especially malignant disease, in order to determine appropriate surgical management.
Here, we report the clinical history of a patient who was suspected to have a follicular thyroid carcinoma (cytology and US findings) with concomitant (incidental) hPTH. A 99mTc-Sestamibi scan identified an area of increased mitochondrial activity (suggesting parathyroid involvement), overlying an area already reported by US, in the right thyroid lobe.
Unequivocally, the surgery should have been the final decision because of hPTH but, in this particular patient, the US and 99mTc-Sestamibi scans were discordant on the tissue origin and the cytological diagnosis was wrong.
Conclusion
Imaging in patients with primary hyperparathyroidism has been proven difficult. We suggest that the combination of 99mTc-Sestamibi scintigraphy, and US may be more informative in such cases.
US, although operator dependent, is relatively cheap and should be carried out first in order to examine the thyroid morphology, the in situ parathyroid glands, when visible, and as a guide for the cytologist. A 99mTc-Sestamibi scan is necessary to detect extra-situ parathyroid glands and to characterize thyroid and parathyroid nodules.
References
1. Udelsman R, Donovan PI and Sokoll LJ (2000) One hundred consecutive minimally invasive parathyroid exploration Ann Surg 232 331–9 PMID 10973383 doi: 10.1097/00000658-200009000-00005
2. Yamashita H, Ohshima A, Uchino S, Watanabe S, Yamashita H and Noguchi S (2000) Endoscopic parathyroidectomy using quick intraoperative intact parathyroid hormone assay J Clin Surg 55 767–9
3. Thompson GB, Mullan BP, Grant CS, Gorman CA, van Heerden JA, O'Connor MK, Goellner JR and Ilstrup DM (1994) Parathyroid imaging with technetium-99m-sestamibi: an initial institutional experience Surgery 116 966–72 PMID 7985104
4. Caixas A, Berna L, Piera J, Rigla M, Matias-Guiu X, Farrerons J and Puig-Domingo M (1995) Utility of 99mTc-sestamibi scintigraphy as a first-line imaging procedure in the preoperative evaluation of hyperparathyroidism Clin Endocrinol (Oxf) 43 525–30 PMID 8548935 doi: 10.1111/j.1365-2265.1995.tb02915.x
5. Howe JR (2000) Minimally invasive parathyoid surgery Surg Clin North Am 80 1399–426 PMID 11059711 doi: 10.1016/S0039-6109(05)70236-X
6. Coakley AJ, Kettle AG, Wells CP, O'Doherty MJ and Collins RE (1989) 99Tcm sestamibi—a new agent for parathyroid imaging Nucl Med Commun 10 791–4 PMID 2532313 doi:10.1097/00006231-198911000-00003
7. Hetrakul N, Civelek AC, Stagg CA and Udelsman R (2001) In vitro accumulation of technetium-99m-sestamibi in human parathyroid mitochondria Surgery 130 1011–8 PMID 11742331 doi: 10.1067/msy.2001.118371
8. O'Doherty MJ, Kettle AG, Wells P, Collins RE and Coakley AJ (1992) Parathyroid imaging with technetium-99m-sestamibi: preoperative localization and tissue uptake studies J Nucl Med 33 313–8 PMID 1531500
9. Rossitch JC, Cowan RJ, Ellis MB and Griffith RF (1995) Tc-99m sestamibi for detection of parathyroid adenoma. Comparison of single and dual tracer imaging Clin Nucl Med 20 220–1 PMID 7750214 doi: 10.1097/00003072-199503000-00006
10. Rubello D, Toniato A, Pelizzo MR and Casara D (2000) Papillary thyroid carcinoma associated with parathyroid adenoma detected by pertechnetate-MIBI subtraction scintigraphy Clin Nucl Med 25 898–900 PMID 11079587 doi: 10.1097/00003072-200011000-00008
11. Gilat H, Cohen M, Feinmesser R, Benzion J, Shvero J, Segal K, Ulanovsky D, and Shpitzer T (2005) Minimally invasive procedure for resection of a parathyroid adenoma: the role of preoperative high-resolution ultrasonography J Clin Ultrasound 33 283–7 PMID 16134156 doi: 10.1002/jcu.20131
12. Erbil Y, Barbaros U, Yanik BT, Salmaslioglu A, Tunaci M, Adalet I, Bozbora A and Ozarmagan S (2006) Impact of gland morphology and concomitant thyroid nodules on preoperative localization of parathyroid adenomas Laryngoscope 116 580–5 PMID 16585862 doi: 10.1097/01.MLG.0000203411.53666.AD
13. Sukan A, Reyhan M, Aydin M, Yapar AF, Sert Y, Canpolat T and Aktas A (2008) Preoperative evaluation of hyperparathyroidism: the role of dual-phase parathyroid scintigraphy and ultrasound imaging Ann Nucl Med 22 123–31 PMID 18311537 doi: 10.1007/s12149-007-0086-z
14. Barczynski M, Golkowski F, Konturek A, Buziak-Bereza M, Cichon S, Hubalewska-Dydejczyk A, Huszno B and Szybinski Z (2006) Technetium-99m-sestamibi subtraction scintigraphy vs. ultrasonography combined with a rapid parathyroid hormone assay in parathyroid aspirates in preoperative localization of parathyroid adenomas and in directing surgical approach Clin Endocrinol (Oxf) 65 106–13 PMID 16817828 doi: 10.1111/j.1365-2265.2006.02556.x
15. Stark DD, Clark OH, Gooding GA and Moss AA (1983) High resolution ultrasonography and computed tomography of thyroid lesins in patients with hyperparathyroidism Surgery 94 863–8 PMID 6648798
16. Regal M, Paramo C, Luna Cano R, Perez Mendez LF, Sierra JM, Rodriguez I and Garcia-Mayor RV (1999) Coexistence of primary hyperparathyroidism and thyroid disease J Endocrinol Invest 22 191–7 PMID 10219886
17. Mihai R, Simon D and Hellman P (2009) Imaging for primary hyperparathyroidism—an evidence-based analysis Langenbecks Arch Surg 394 765–84 PMID 19590890 doi: 10.1007/s00423-009-0534-4
18. Lever EG, Refetoff S, Straus FH 2nd, Nguyen M and Kaplan EL (1983) Coexisting thyroid and parathyroid disease—are they related? Surgery 94 893–900 PMID 6648801
19. dell'Erba L, Baldari S, Borsato N, Bruno G, Calò-Gabrieli G, Carletto M et al (2001) Retrospective analysis of the association of nodular goiter with primary and secondary hyperparathyoidism Eur J Endocrinol 145 429–34 PMID 11581000 doi: 10.1530/eje.0.1450429
20. Burmeister LA, Sandberg M, Carty SE and Watson CG (1997) Thyroid carcinoma found at parathyroidectomy: association with primary, secondary, and tertiary hyperparathyroidism Cancer 79 1611–6 PMID 9118047 doi: 10.1002/(SICI)1097-0142(19970415)79:83.0.CO;2
21. Maiorano E, Ambrosi A, Giorgino R, Fersini M, Pollice L and Ciampolillo A (1994) Insulin-like growth factor 1 (IGF-1) in multinodular goiters: a possible pathogenetic factor Pathol Res Pract 190 1012–6 PMID 7746734
22. McCarty MF (2000) Parathyroid hormone may be a cancer promoter—an explanation for the decrease in cancer risk associated with ultraviolet light, calcium, and vitamin D Med Hypothesis 54 475–82 PMID 10783492 doi: 10.1054/mehy.1999.0880
23. Masatsugu T, Yamashita H, Noguchi S, Nishii R, Koga Y, Watanabe S et al (2005) Thyroid evaluation in patients with primary hyperparathyroidism Endocrinol J 52 177–82 PMID 15863944






