Gastric cancer, one of the leading causes of cancer-associated mortality worldwide, is renowned for its ability to disseminate throughout the peritoneal cavity.
As well as causing secondary tumours in other organs, metastatic gastric cancer cells trigger extensive stromal fibrosis, or the formation of scar tissue, that can be more deadly than the cancer itself--bowel obstruction and hydronephrosis and jaundice are all common side effects of gastric cancer-associated fibrosis.
What's more, the densely packed scar tissue can disturb chemotherapy drugs from reaching their target due to intra-tumoural high pressure.
Preventing fibrosis could therefore improve the prognosis for gastric cancer patients. The problem is, researchers have yet to discover what causes fibrosis, let alone how to prevent it.
But in a study published recently in Gastric Cancer, researchers from Kanazawa University found that an inflammatory protein produced by mast cells, IL-17A, triggers cellular changes in the peritoneum, leading to stromal fibrosis in gastric cancer patients.
Lead author Katsuya Gunjigake from Kanazawa University's Division of Cancer Medicine explains why the researchers targeted IL-17A.
"Over-stimulation of the immune system by IL-17A plays a major role in chronic inflammatory diseases such as rheumatoid arthritis and multiple sclerosis.
It has also been associated with increased tumour growth and dissemination in various forms of cancer.
Interestingly though, while studies had shown that IL-17A causes fibrosis in both Crohn's disease and lung disease, no one had investigated the link between tissue fibrosis and IL-17A in cancer."
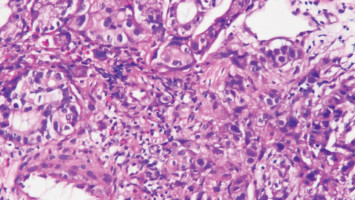
By studying cancerous tissue from 70 gastric cancer patients with peritoneal dissemination, the researchers discovered that the degree of fibrosis was governed by the amount of IL-17A, and that IL-17A was being produced by a subgroup of white blood cells called mast cells.
Says Gunjigake, "Mast cells are most commonly associated with anaphylaxis but are also involved in pathogen defence and immune tolerance, among other things. They contain small particles called granules that are filled with molecules such as histamine, serotonin, and IL-17A that are released into the extracellular environment in a process known as degranulation."
The researchers then injected mice with human peritoneal cells and gastric cancer cells and examined the effects of IL-17A treatment, with interesting results.
"Not only did IL-17A increase tumour size and the degree of fibrosis, it also changed the structure of the peritoneal cells, enhancing their invasive and migratory capabilities," explains responsible author Sachio Fushida.
"Given the obvious role of IL-17A in driving fibrosis, our results suggest that suppression of mast cell degranulation may be a promising treatment strategy for gastric cancer patients with peritoneal dissemination."
Source: Kanazawa University
The World Cancer Declaration recognises that to make major reductions in premature deaths, innovative education and training opportunities for healthcare workers in all disciplines of cancer control need to improve significantly.
ecancer plays a critical part in improving access to education for medical professionals.
Every day we help doctors, nurses, patients and their advocates to further their knowledge and improve the quality of care. Please make a donation to support our ongoing work.
Thank you for your support.