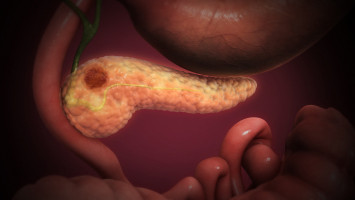
Patients with metastatic pancreatic cancer who had germline or somatic mutations in DNA repair genes had better clinical outcomes after platinum-based chemotherapy, as compared with patients without these mutations, according to a study published in Clinical Cancer Research, a journal of the American Association for Cancer Research
Metastatic pancreatic cancer is associated with a challenging prognosis with a relative five-year survival rate of 2.9 percent.
The current standard of care for metastatic pancreatic cancer includes platinum-based chemotherapy.
"Unfortunately, there are no validated biomarkers to predict which patients might benefit from standard treatment," said senior author was Eileen O'Reilly, MD, medical oncologist at Memorial Sloan Kettering Cancer Center (MSKCC).
Biomarkers are biological features, such as DNA mutations, that can be used to predict prognosis or response to treatment.
DNA mutations may be found in one or both copies of the gene.
Furthermore, mutations may be germline mutations, which are inherited and are found in every cell of the body, or they may be somatic, which arise after conception and are not found in every cell.
Approximately 5 to 9 percent of patients with pancreatic cancer have germline or somatic mutations in the BRCA1, BRCA2, and/or PALB2 genes, according to O'Reilly.
The proteins encoded by these genes are involved in a form of DNA repair known as homologous recombination (HR).
Results from recent clinical trials showed that patients with germline mutations in BRCA1, BRCA2, and/or PALB2 had clinical responses to platinum-based chemotherapy or the PARP inhibitor olaparib.
"These studies demonstrate that germline mutations in BRCA1, BRCA2, or PALB2 are valuable biomarkers to predict response to treatment," said lead author Wungki Park, MD, medical oncologist at MSKCC. "This led us to ask whether the benefit was limited to germline mutations only, or whether somatic mutations in these genes or mutations in other HR genes are also associated with responses to platinum-based chemotherapy."
In this study, Park, O'Reilly, and colleagues analysed the association between mutations in HR genes and clinical outcome.
The study included 262 patients with metastatic pancreatic cancer, who underwent both germline and somatic sequencing using the MSK-IMPACT sequencing test.
The researchers analysed 17 HR genes included in both the somatic and germline panels of the MSK-IMPACT gene set.
Analysis of sequencing data allowed the researchers to determine whether mutations were germline or somatic, in core HR genes (BRCA1, BRCA2, or PALB2) or in noncore HR genes (such as ATM, CHEK2, BAP1, RAD51, FANCA, and 9 others), and in one or both copies of each gene.
Out of 262 patients, 50 patients had mutations in HR genes; 40 patients had germline mutations, and 10 had somatic mutations.
Thirty-one patients had mutations in core genes, while 19 patients had mutations in noncore genes.
Twenty-nine patients had mutations in both copies of a gene, and 21 patients had mutations in only one gene copy.
The median overall survival for the entire cohort of 262 patients was 15.5 months.
Overall survival was similar between patients with germline mutations and those with somatic mutations.
Thus, these subgroups were combined in the ensuing analyses.
The authors found that for the 35 patients who were treated with first-line platinum-based chemotherapy, those with mutations in HR genes had greater overall survival compared with those without mutations in these genes (25.1 months vs. 15.3 months), suggesting that mutations in HR genes may be associated with enhanced overall survival.
Furthermore, patients with HR mutations had a 44 percent lower risk of disease progression than patients without these mutations after first-line treatment with platinum-based chemotherapy.
The lower risk of disease progression was observed regardless of whether the mutations were in core or noncore HR genes.
Among patients with mutations in HR genes, those who were treated with platinum-based chemotherapy had higher progression-free survival (PFS) than those who received non-platinum treatment (12.6 months vs. 4.4 months).
For the patients with mutations in both gene copies, those who were treated with platinum-based chemotherapy had greater PFS than those treated with other therapies (13.3 months vs. 3.8 months).
This association was not observed for patients with mutations in only one gene copy, suggesting that platinum-based chemotherapy may provide a greater clinical benefit in patients with mutations in both copies of HR genes.
"Our data support the use of platinum-based chemotherapy as first-line treatment for patients with defects in various HR genes," said O'Reilly. "The results underscore the importance of genetic testing in newly diagnosed patients to help refine treatment decisions."
"HR deficiency defined by pathogenic mutation of core HR genes and loss of both copies of either core or noncore HR genes confers the greatest platinum sensitivity," said Park. "Patients with these deficiencies represent the optimal subgroup for therapies that target DNA repair pathways, such as platinum-based chemotherapy."
He noted that these deficiencies could also be predictive of response to other targeted developmental therapeutics in DNA repair pathways, to other PARP inhibitors, and to immunotherapy, although additional research into these will be needed.
"Identifying factors associated with treatment response may also help us understand why some patients' tumours do not respond to treatment and why some that respond ultimately develop resistance," Park added.
A limitation of the study is that the analysis was performed on a highly selected group of patients and therefore may not represent all patients with pancreatic cancer.
"While the data are very compelling, we need to validate the results prospectively in wider and larger datasets," noted O'Reilly.
Additional challenges included low sample purity, limited tissue availability, and other technical limitations.
We are an independent charity and are not backed by a large company or society. We raise every penny ourselves to improve the standards of cancer care through education. You can help us continue our work to address inequalities in cancer care by making a donation.
Any donation, however small, contributes directly towards the costs of creating and sharing free oncology education.
Together we can get better outcomes for patients by tackling global inequalities in access to the results of cancer research.
Thank you for your support.