Why do some cancers come back?
Sometimes, a treatment can effectively eliminate cancer cells to undetectable levels, but, if the treatment stops, cancer may return.
This is the case of chronic myeloid leukaemia treated with drugs known as tyrosine kinase inhibitors.
These drugs have dramatically improved clinical outcomes and generated unprecedented rates of complete responses and long term survival.
To achieve these results, patients have to take the drug for the rest of their lives.
"Clinical trials testing the effect of discontinuing the drug have shown that at least half of the patients achieve treatment-free remission, but in the other half the cancer returns," said Dr Daniel Lacorazza, associate professor of pathology & immunology at Baylor College of Medicine and principal investigator in the Experimental Immunology & Hematology Laboratory at Texas Children's Hospital. "We think that relapse occurs because tyrosine kinase inhibitors affect most chronic myeloid leukaemia cells, but not leukaemia stem cells. It's like removing the tree, but leaving the roots that can sprout new shoots."
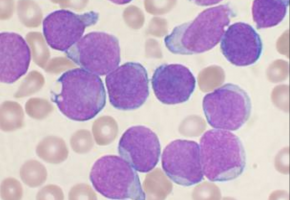
Leukaemia stem cells are an elusive, small cell population that initiates and sustains leukaemia.
Stem cells can regenerate via a poorly understood mechanism of self-renewal and enter a path of development that gives rise to new leukaemia cells.
Lacorazza and his colleagues think that clues to treatment-free remission might be found in this little known, self-renewal mechanism.
"The results of the drug discontinuation trials suggest that a cure may not be possible with tyrosine kinase inhibitors alone. We think that new breakthroughs in chronic myeloid leukaemia therapy may emerge from the identification of novel mechanisms of leukaemia stem cell self-renewal and the development of drugs that specifically target these mechanisms," said Lacorazza, who also is member of the Dan L Duncan Comprehensive Cancer Center at Baylor.
Patient consensus supports the search for novel treatments for leukaemia stem cells that would eliminate the leukaemia without having to take the drug for life and managing side effects.
Treatment-free remissions would also reduce the emotional and financial burdens in a growing population of chronic myeloid leukaemia patients in lifelong therapy.
Unraveling clues of leukaemia stem cell self-renewal
Lacorazza and his colleagues wanted to improve their understanding of how leukaemia stem cells renew themselves.
Their goal was to identify a step in the process that could be manipulated to lead to the elimination of leukaemia stem cells and the prevention of relapses.
"In my laboratory, we have been working with mouse models to study the leukaemia stem cell population in chronic myeloid leukaemia. Specifically, we have investigated the role KLF4 plays on leukaemia stem cell self-renewal," Lacorazza said.
KLF4, or Krüppel-like factor 4, is a transcription factor known to be essential in the self-renewal of other cell types, such as embryonic stem cells, and also in other types of cancer.
"We found that removing the KLF4 gene from leukaemia stem cells in our mouse model resulted in unstable stem cells that were spontaneously lost and consequently the mice remained free of leukaemia," Lacorazza explained. "We also conducted molecular studies to explore the mechanism behind this result. A major change in the absence of KLF4 was an increase in the production of kinase DYRK2, an enzyme involved in protein stability, cell cycle control and apoptosis (programmed cell death)."
The findings, published in the journal Blood, suggested that KLF4 promotes disease progression in this mouse model by repressing the production of the DYRK2 enzyme.
The results also suggested that it was possible that doing the opposite, elevating the production of DYRK2 enzyme, would reduce or inhibit leukaemia stem cell survival and self-renewal.
Looking to translate these results to the clinic, the researchers searched for a possible pharmacological means to enhance the stability of the DYRK2 enzyme.
Searching the literature revealed a potential way to achieve this goal.
They found that vitamin K3 inhibits SIAH2, an enzyme that is implicated in the degradation of DYRK2.
"We hypothesised that if we inhibited SIAH2 with vitamin K3, we would prevent or reduce the degradation of DYRK2, and therefore likely increase the levels of DYRK2, which would trigger inhibition of survival and self-renewal of leukaemia stem cells," Lacorazza said.
The researchers tested this strategy in chronic myeloid leukaemia cell lines, in their mouse model and in patient samples in the lab.
The results were encouraging.
They saw that treatment with vitamin K3 increased DYRK2 and inhibited the expansion of the leukaemia stem cells.
Looking for the right drug
"Vitamin K3 may be toxic to humans. Although in our view vitamin K3 is not going to be the drug to treat leukaemia stem cells, it has proved the concept that stabilizing DYRK2 enzyme could help eliminate the leukemic stem cell population," Lacorazza said.
Lacorazza and his colleagues are currently searching for drugs that could eliminate leukaemia stem cells safely in patients.
"We envision that targeting the bulk of leukaemia with tyrosine kinase inhibitors plus a new drug that targets the stem cells might be a future strategy for patients to reach drug-free remission," Lacorazza concluded.
Source: Baylor College of Medicine