A Massachusetts General Hospital (MGH) research team has identified an additional mechanism for resistance to targeted treatment for BRAF-mutant melanoma.
Their paper, receiving advance online publication in Nature Medicine, reports that inactivating mutations in two genes responsible for regulating key aspects of cell division can reactivate the signalling pathway driving tumour growth that had been blocked by BRAF inhibitor drugs.
"Our finding that loss of the tumour suppressors STAG2 or STAG3 is a novel genetic mechanism of BRAF inhibitor resistance also revealed an unexpected link between those proteins and the MAPK cell-growth pathway, activation of which drives these tumours," says Bin Zheng, PhD, of the Cutaneous Biology Research Center at MGH, corresponding author of the paper. "Understanding and overcoming resistance to BRAF inhibition remains a major challenge facing the melanoma field. Indentifying biomarkers capable of predicting response to BRAF inhibitor drugs - such as vemurafenib and dabrafenib - will facilitate early identification of patients likely to benefit from treatment and enable monitoring the development of resistance, which would allow consideration of other treatment options prior to relapse."
In about half the cases of malignant melanoma - the most deadly form of skin cancer - tumour growth is driven by mutations in the BRAF gene, and treatment of those tumours with drugs that inhibit BRAF activity can reverse tumour growth in most cases.
But treatment resistance almost invariably develops, leading to a resumption of tumour growth.
Several mechanisms behind this resistance have been identified, including mutations in other genes in the MAPK pathway, of which BRAF is a component, which essentially circumvents the suppression of BRAF activity.
But as many as 25 percent of cases of resistance to BRAF inhibitors do not involve identified mechanisms.
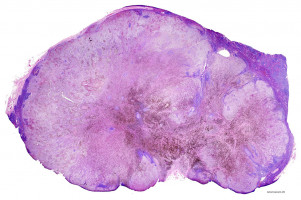
In their search for additional resistance mechanisms, the investigators first performed whole-exome sequencing of a patient's tumour samples taken before treatment and after the development of resistance to the BRAF inhibitor vemurafinib.
A comparison of novel mutations in the post-resistance sample with a list of known cancer-associated mutations identified a single significant mutation in the tumour suppressor STAG2.
That gene and related genes called STAG1 and STAG3 code for subunits of the cohesin complex, an assembly of proteins that regulates an essential stage in cellular division - the separation of chromosomes - and also may play a role in the regulation of gene expression.
Several cohesin complex genes, including STAG2, are known to be mutated in other forms of cancer.
Zheng notes that exactly how the proteins exert their tumour suppressor functions in any type of cancer has yet to be determined.
Examination of the levels of all three STAG proteins in a panel of treatment-resistant melanoma cell lines identified reduced expression of STAG2 and STAG3 in several lines, including some that were resistant to inhibition of both BRAF and of MEK, another protein in the MAPK pathway.
They identified what may be the responsible STAG2 mutation, and while they could not find any STAG3 mutation in their panel, examination of data from a previously published study of BRAF inhibitor treatment identified STAG3 mutations in pretreatment samples of tumours that soon developed resistance to treatment.
Experiments in cultured melanoma cell lines and in tumours implanted into mice revealed that knockdown of the expression of either protein reduced sensitivity to BRAF inhibition by reactivating a later stage of the MAPK pathway.
In contrast, increasing the expression of either STAG2 or STAG3 in BRAF-mutated melanoma cells increased the effectiveness of vemurafinib treatment.
"The observation that mutations of STAG2 or STAG3 can lead to reactivation of the MAPK pathway was a novel and unexpected finding of our study," says Zheng, who is an assistant professor of Dermatology at Harvard Medical School. "We are now working to identify vulnerabilities in STAG2/3 mutant melanomas and discover new approaches to targeting these tumours, which we hope will provide new insight into both preventing BRAF inhibitor resistance and treating tumours that have become resistant."
Source: Massachusetts General Hospital
The World Cancer Declaration recognises that to make major reductions in premature deaths, innovative education and training opportunities for healthcare workers in all disciplines of cancer control need to improve significantly.
ecancer plays a critical part in improving access to education for medical professionals.
Every day we help doctors, nurses, patients and their advocates to further their knowledge and improve the quality of care. Please make a donation to support our ongoing work.
Thank you for your support.