Researchers from the Cancer Science Institute of Singapore (CSI Singapore) at the National University of Singapore (NUS) have identified a set of genes, including DNMT3A, that could potentially be used to predict clinical outcomes of patients who suffer from a type of Acute Myeloid Leukemia (AML) associated with an FLT3 internal tandem duplication (FLT3-ITD) mutation.
Specifically, the research team led by Professor H. Phillip Koeffler, Senior Principal Investigator at CSI Singapore, found that chemotherapy may cause certain genes to mutate further in patients with FLT3-ITD AML.
Researchers also identified DNMT3A as a potential marker for monitoring patient’s chemotherapy response since patients with this mutation during remission tend to have short relapse-free survival and low overall survival rates.
The findings, which were published online in Blood, a medical journal published by the American Society of Hematology, contribute to the understanding of the underlying molecular causes of FLT3-ITD AML and present opportunities for scientists to develop effective targeted therapies.
Poor clinical outcomes associated with FLT3-ITD AML
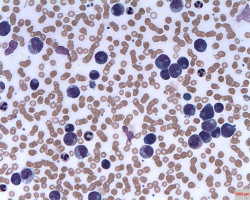
AML is a blood cancer characterised by the rapid growth of abnormal white blood cells, and its incidence increases with age.
AML arises as a result of acquired or inherited DNA mutations.
About 20 to 30 per cent of AML patients have a type of genetic mutation called FLT3-ITD, which encourages aberrant growth of cancer cells.
The prognosis for this subgroup of patients is commonly associated with poor clinical outcome and increased relapse rates.
Although 70 per cent of FLT3-ITD AML patients achieve a complete remission with conventional chemotherapy, the majority of these patients eventually relapse and die of therapy-resistant leukaemia.
Therefore, there is an urgent a need to identify genomic abnormalities underlying this AML subtype both at diagnosis and relapse to help scientists better understand this disease.
The research team at CSI Singapore, tested 80 patient samples to uncover the mutational spectrum associated with the relapse of the disease.
The team searched for mutations on genes which are essential for cell maintenance and identified a set of genes, specifically DNMT3A, to be recurrently mutated.
DNMT3A as a genetic marker for more effective screening of AML patients for targeted treatment
“The findings from this study suggest that chemotherapy may have induced further gene mutations in patients with FLT3-ITD AML, which eventually causes majority of these patients to eventually suffer from relapse and develop therapy-resistant leukaemia with poor survival rate. Specifically, we found that DNMT3A mutations are the most stable mutations. Therefore, patients who have undergone chemotherapy can test for the presence of DNMT3A mutations through the testing of blood samples to determine if the cancerous cells are still present and the likelihood of a relapse. It can also serve as a marker at the point of diagnosis for the selection of appropriate treatment,” said Prof Koeffler.
In addition, the study also identified a number of novel genes that contribute to leukaemia and these findings may serve as a basis for further investigation into potential treatment avenues for AML.
Prof Koeffler and his team are currently delving deeper into the potential role and mechanisms of the identified genes in causing leukaemia.
Source: National University of Singapore
The World Cancer Declaration recognises that to make major reductions in premature deaths, innovative education and training opportunities for healthcare workers in all disciplines of cancer control need to improve significantly.
ecancer plays a critical part in improving access to education for medical professionals.
Every day we help doctors, nurses, patients and their advocates to further their knowledge and improve the quality of care. Please make a donation to support our ongoing work.
Thank you for your support.