Patients with anaplastic glioma without 1p/19q co-deletion benefit from adjuvant chemotherapy, according to early results from a European phase III trial.
The estimated five-year survival rates were 56% with radiation therapy and adjuvant temozolomide versus 44% without adjuvant temozolomide.
The addition of adjuvant temozolomide also delayed disease progression by more than two years.
The study was featured in a press briefing and presented at the 2016 American Society of Clinical Oncology (ASCO) Annual Meeting.
“Until this study, doctors had no evidence to support the use of adjuvant temozolomide in patients with grade III anaplastic glioma,” said lead study author Martin J. van den Bent, MD, a professor of neuro-oncology at Erasmus MC Cancer Center in Rotterdam, The Netherlands.
“These findings should expand treatment choices and change the way we treat patients with this rare form of brain cancer.”
About the Study
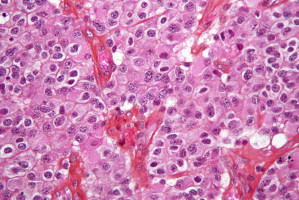
Co-deletion of chromosome arms 1p and 19q occurs in a specific type of brain cancer.
Patients who have this genetic abnormality tend to respond better to chemotherapy and live longer.
The Concurrent and Adjuvant Temozolomide Chemotherapy in Non-1p/19q Deleted Anaplastic Glioma (CATNON) trial was limited to patients who lack 1p/19q co-deletion (a separate trial focuses on patients who have this marker).
Researchers randomly assigned 748 patients to four different treatment groups:
• Radiation therapy alone
• Temozolomide during radiation therapy
• Temozolomide during and after radiation therapy
• Temozolomide after radiation therapy (adjuvant temozolomide)
The study was conducted by the European Organisation for Research and Treatment of Cancer (EORTC) and enrolled patients in 118 institutions in Europe, North America, and Australia.
Key Findings
Patients who received temozolomide after radiation therapy with or without concurrent temozolomide had slower disease progression than those treated without adjuvant therapy.
The median time to disease progression was more than double in the adjuvant temozolomide group (42.8 months vs. 19 months).
The median overall survival has not been reached in patients treated with adjuvant temozolomide.
Long-term survival estimates also support the use of adjuvant temozolamide; 56% of patients were alive at five years with adjuvant temozolomide compared to 44% with radiation therapy alone or with temozolomide given during radiation therapy.
The results of the temozolomide treatment given only during radiation therapy are not yet available and final data from this study are expected in 2020.
Temozolomide is an oral drug and is generally well tolerated by patients.
The most common toxicities in the temozolomide study arms were mainly haematologic (e.g., low platelets and white blood cells), with severe toxicity in 5 - 10% of patients.
Next Steps
Future research will focus on identifying patients who are most likely to benefit from adjuvant temozolomide.
The researchers plan to assess or re-examine additional genetic abnormalities known to affect prognosis in this cancer: MGMT promotor methylation and IDH mutation.
Watch the press conference and video interview for more.
Source: ASCO
The World Cancer Declaration recognises that to make major reductions in premature deaths, innovative education and training opportunities for healthcare workers in all disciplines of cancer control need to improve significantly.
ecancer plays a critical part in improving access to education for medical professionals.
Every day we help doctors, nurses, patients and their advocates to further their knowledge and improve the quality of care. Please make a donation to support our ongoing work.
Thank you for your support.