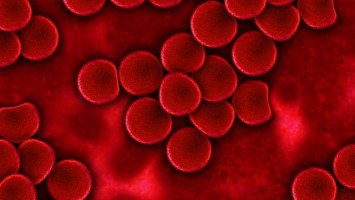
Building upon previous research, scientists at University of California, San Diego School of Medicine and UC San Diego Moores Cancer report that a protein called Wnt5a acts on a pair of tumour-surface proteins, called ROR1 and ROR2, to accelerate the proliferation and spread of chronic lymphocytic leukaemia (CLL) cells, the most common form of blood cancer in adults.
They note, however, that these effects of Wnt5a were blocked by a humanised monoclonal antibody specific for ROR1, called cirmtuzumab (or UC-961), which inhibited the growth and spread of CLL cells in both cell lines and mouse models of leukaemia.
The findings are published in the Dec. 21, 2015 issue of The Journal of Clinical Investigation.
Although the findings are made with leukaemia cells, researchers said the study has implications for patients with other cancers, including solid-tissue tumours.
ROR1 and ROR2 are considered 'orphan receptors,' which are expressed primarily during embryonic development.
The expression of these proteins, particularly ROR1, becomes suppressed during foetal development and is negligible on normal adult tissues.
However, CLL and many solid tissue cancers re-express these orphan receptors.
"Our findings show that ROR1 and ROR2 team up to stimulate tumour cell growth and metastasis in response to Wnt5a, which appears over-expressed in patients with CLL and can act as a survival/growth factor for leukaemia cells. By blocking the capacity of Wnt5a to stimulate tumour cells, cirmtuzumab can inhibit the growth and spread of cancer cells," said senior author Thomas J. Kipps, MD, PhD, Evelyn and Edwin Tasch Chair in Cancer Research and deputy director for research at Moores Cancer Center.
"We now have better insight into how cirmtuzumab works against leukaemia cells. This should help find better ways to treat patients who have other cancers with cirmtuzumab, which currently is being evaluated in a phase I clinical trial for patients with CLL."
The JCI paper follows a series of fundamental findings published by Kipps and colleagues in recent years:
In 2008, they reported that patients vaccinated with their own leukaemia cells could make antibodies against ROR1, some of which had the ability to reduce the survival of leukaemia cells.
They found ROR1 on leukaemia cells but not on all normal adult tissues examined.
In 2012, they reported finding ROR1 on many different types of cancer, particularly cancers that appear less differentiated and more likely to spread to other parts in the body.
Because this protein was not found on normal adult tissues, these findings made ROR1 a new target for anti-cancer drug research.
LIn June 2013, they linked ROR1 to a process used in early development, suggesting cancer cells hijack an embryological process – called epithelial-mesenchymal transition – to spread or metastasize more quickly.
In January 2014, they reported expression of ROR1 resulted in a faster-developing, more aggressive form of CLL in mice.
In September 2014, they launched a phase 1 human clinical trial of a new monoclonal antibody for patients with CLL.
The drug, called cirmtuzumab, targets ROR1 in cancer cells in general and cancer stem cells in particular.
The safety trial is on-going.
In November 2014, they described cellular experiments indicating cirmtuzumab might also be effective against cancer stem cells, which appear responsible for the relapse and spread of cancer after conventional therapy.
The latest research more precisely defines the critical roles of ROR1 and ROR2 in cancer development.
Both are evolutionarily conserved proteins, found in many species, and most active in the early stages of embryogenesis, when cells are migrating to form organs and parts of the body.
The lack of either during this process results in severe developmental abnormalities.
Low levels of ROR2 remain in some adult tissues, but ROR1 is found only in cancer cells.
Researchers found that in response to signalling by Wnt5a, ROR1 and ROR2 come together to signal the growth and migration of cancer cells.
Such migration contributes to the spread of cancer to cause metastasis, which is responsible for 90 percent of cancer-related deaths.
But treating mice with cirmtuzumab disrupted the process, inhibiting engraftment of leukaemia cells and slowing or stopping the disease from spreading.
We are an independent charity and are not backed by a large company or society. We raise every penny ourselves to improve the standards of cancer care through education. You can help us continue our work to address inequalities in cancer care by making a donation.
Any donation, however small, contributes directly towards the costs of creating and sharing free oncology education.
Together we can get better outcomes for patients by tackling global inequalities in access to the results of cancer research.
Thank you for your support.