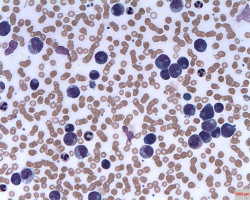
Adjusting the intensity of treatment based on the patient’s likelihood of relapse has emerged as a promising strategy for treating children with acute lymphocytic leukaemia (ALL).
This is the first Children’s Oncology Group (COG) study to systematically assess minimal residual disease at the end of induction therapy and use this, in concert with clinical and biological data, for risk stratification and treatment assignment.
Newly diagnosed B-cell lymphocytic leukaemia patients between one and 30 years of age received either standard or high-risk initial chemotherapy regimens based on the National Cancer Institute’s (NCI) definitions of these risks.
Patients underwent standardised testing to detect cytogenetic abnormalities associated with favourable and unfavourable outcomes.
Investigators classified 5,104 NCI standard risk (SR) and 2,791 NCI high risk (HR) patients into low, standard, high, or very high risk groups at the end of induction therapy based on the presence of favourable and unfavourable cytogenetic findings and early treatment response.
The investigators determined that the five-year event-free survival varies according to genetic subset, ranging from 70 percent for those with unfavourable cytogenetics to 95 percent for those with favourable cytogenetic abnormalities.
Notably, patients with either standard or high-risk disease and favourable cytogenetic findings, who accounted for almost half of all patients, had a 98 percent likelihood of being alive five-years following diagnosis.
Results demonstrate that this real-time classification identified a previously unrecognised subset of high risk patients with excellent chances for cure without further intensification of treatment.
Watch the press conference and watch the video interview for more information.
Source: ASH