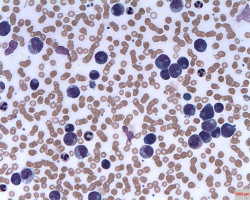
A new study reveals that insurance status, marital status, and county-level income may affect the chances of survival in young patients with acute myelogenous leukaemia (AML).
Published early online in Cancer, a peer-reviewed journal of the American Cancer Society, the findings indicate that efforts are needed to address the social factors that impact critical aspects of health in these patients.
AML will affect approximately 20,830 and kill 10,460 Americans in 2015.
Tremendous progress has been made in identifying disease characteristics that cause a patient to have a higher or lower chance of cure following intense treatment, which often involves bone marrow transplantation.
Now investigators at the University of Alabama at Birmingham have analysed a database with 5,541 patients younger than 65 years of age to demonstrate that, in addition to age and disease characteristics, other “non-biological” patient characteristics also matter.
The study is the largest to date to look at socioeconomic factors in outcomes of younger patients with AML.
Patients who were single or divorced, patients who were uninsured or were Medicaid beneficiaries, and patients who lived in areas with lower income had substantially elevated risks of dying prematurely.
“We believe these three factors indicate lack of material and social support preventing young patients from successfully walking the long and difficult road towards a cure,” said Uma Borate, MD, lead author of the study, and assistant professor in the UAB Division of Haematology and Oncology.
The findings show that factors not necessarily related to care can have significant impacts on AML patients’ outcomes.
“As physicians, we often emphasise more of the biology of the cancer, especially with the recent focus on personalised medicine.
But we need to pay the same attention to resources available to our patients, as this greatly impacts their chances to survive leukaemia,” said senior author Luciano Jose Costa, MD, PhD, associate professor in the UAB Division of Haematology and Oncology.
This will be especially important as the U.S. transitions to a healthcare system that ties physician and hospital payments to patient outcomes.
“Taking from the results of this study, factors that have nothing to do with quality of care need to be accounted for when comparing predicted with actual outcomes--otherwise we will create a disincentive for hospitals and doctors to care for less privileged patients,” said Dr Borate.
Source: Cancer