by ecancer reporter Janet Fricker
A new blood based marker engineered to detect a broad spectrum of tumours demonstrated efficacy in mice, reports a study in PNAS.
The system, suggest the US authors, offers an ‘alternative paradigm’ for improved cancer detection to enable more timely interventions.
The time at which cancers are detected, both at initial diagnosis and during recurrence, represents one of the most important factors influencing outcomes.
The majority of cancers are detected late, with an adverse effect on mortality.
Strategies to improve detection have included the development of assays identifying endogenous cancer biomarkers shed into the blood stream.
But while various tumour types secrete biomarkers into the blood, biomarkers are typically specific to one type of tumour requiring separate testing.
Additional obstacles include low blood biomarker concentrations, rapid biomarker degradation and highly variable background expression of the biomarker in non-malignant tissues.
To overcome limitations of endogenous biomarker detection, Sanjiv Gambhir and colleagues, from Stanford University, California, have devised an alternative strategy based on the identification of tumour-bearing individuals using a blood-based detection system of exogenously delivered, genetically encoded reporters producing tumour driven biomarkers.
The team engineered DNA ‘minicircles’, consisting of an artificial single-stranded DNA ring containing a single gene coding for secreted embryonic alkaline phosphatase (SEAP) and a short DNA sequence, known as a promoter, that acts as a ‘switch’.
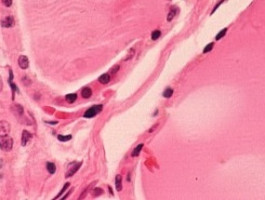
The switch is regulated by a protein called Survivin, a member of the apoptosis inhibitor family, that is known to be expressed in many cancers, including melanoma, liver, lung, breast, colon and ovarian.
Survivin is not expressed at detectable levels in healthy adult tissue.
The result is that SEAP production is only ever turned on in the presence of cancer.
Furthermore, that SEAP is only expressed in embryos means that there should be zero background levels in the blood of healthy adults.
In a mouse model, the investigators found that systemic administration of the ‘mini circles’ enabled them to differentiate between mice bearing human melanoma metastases and tumour-free mice.
In the study they could detect levels of SEAP in the blood from three days to two weeks after the injection, at levels distinguishable from non-tumour bearing mice 92% of the time.
Further studies in mice with lung tumours showed cumulative SEAP levels correlated with lung tumour burden, suggesting SEAP levels could serve an indicator of the extent of disease.
“Continued development of our system could improve tumour detectability dramatically because of the temporally controlled, high reporter expression in tumours and nearly zero back-ground from healthy tissues,” write the authors.
The system, they add, could be used first in patients at high risk for tumour recurrence, followed by screening of populations considered at high risk. If proven safe and effective, they believe the approach could serve as a powerful cancer-screening tool for the general population.
Future improvements in both the vector itself and the delivery of vector to tumours, they add, should make it possible to detect smaller and smaller tumours with time.
Reference
J Ronald, H Chuang, A Dragulescu-Andrasi, et al. 'Detecting cancers though tumor-activatable minicircles that lead to a detectable blood biomarker, PNAS, 2015
The World Cancer Declaration recognises that to make major reductions in premature deaths, innovative education and training opportunities for healthcare workers in all disciplines of cancer control need to improve significantly.
ecancer plays a critical part in improving access to education for medical professionals.
Every day we help doctors, nurses, patients and their advocates to further their knowledge and improve the quality of care. Please make a donation to support our ongoing work.
Thank you for your support.