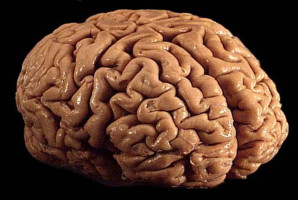
Glioblastoma is the most prevalent and aggressive brain tumour.
It proliferates very rapidly, is highly invasive, and there is currently no treatment capable of halting its progression or curing it, which means life expectancy after diagnosis is very short.
The standard procedure involves surgical resection of the tumour followed by radiotherapy and chemotherapy, but even with this aggressive treatment, recurrences are very common, often within a year.
Now, in an article published in the prestigious journal Advanced Science, a research team led by Professor Víctor Yuste, from the Department of Biochemistry and Molecular Biology and the Institut de Neurociències de la UAB (INc-UAB), has designed and tested several bioadhesive patches that could be placed at the site where the tumour is removed during surgery, targeting any remaining cancer cells.
The design of the patches is inspired by the way mussels adhere to rocks (using polyphenol-type molecules), allowing the material to strongly attach to moist brain tissue and enabling sustained release of the drug.
According to the results, among all the tested options, the patch containing catechin—a natural polyphenol found in green tea, cocoa, and some fruits—performed best, eliminating approximately 90% of malignant cells.
This highly oxidising material induces cell death by increasing reactive oxygen species (ROS).
“If catechin were administered orally, it could cause unwanted systemic side effects. However, by adhering to the area from which the tumour has been removed, it can act locally, minimising or even preventing the appearance of side effects,” explains Professor Yuste.
In addition, “these materials show high antimicrobial activity and excellent biocompatibility, which would help prevent infections and promote proper wound healing. Combined with their extremely low production cost and the simplicity of their fabrication, they represent a viable option in terms of future development, scalability, and potential investor interest,” adds Jose Bolaños-Cardet, a researcher at the UAB and the Catalan Institute of Nanoscience and Nanotechnology (ICN2).
The study, a collaboration among several research centres in Catalonia—including the INc-UAB, the ICN2, and the Bellvitge University Hospital – Catalan Institute of Oncology (ICO) – Bellvitge Biomedical Research Institute (IDIBELL)—could represent a major step forward in the treatment of glioblastoma and offer hope to patients facing this devastating diagnosis.
This project is funded by the Spanish Ministry of Science, Innovation and Universities (MICIU), the State Research Agency (AEI) [10.13039/501100011033], and the European Regional Development Fund (ERDF – EU), within the framework of project PID2024-161159OB-I00.
The World Cancer Declaration recognises that to make major reductions in premature deaths, innovative education and training opportunities for healthcare workers in all disciplines of cancer control need to improve significantly.
ecancer plays a critical part in improving access to education for medical professionals.
Every day we help doctors, nurses, patients and their advocates to further their knowledge and improve the quality of care. Please make a donation to support our ongoing work.
Thank you for your support.