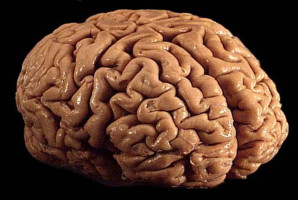
Brain tumours, particularly gliomas, remain challenging to diagnose and treat.
While radiology reports can offer non-invasive insights into tumour size, shape, and progression, with pathology reports providing definitive evidence of cellular and molecular features, the lack of integration between these two information sources often complicates clinical decision-making.
To overcome this, a research team led by Dr. Zhuoqi Ma from the Department of Radiology at Brown University and Brown University Health created a pipeline that employs a pre-trained large language model to unify radiology and pathology reports.
In a sample of 426 patients, the system achieved a micro F1-score of 0.849 for tumour presence and 0.929 for tumour stability, surpassing single-source methods by more than 10%.
“Large language models (LLM) can synthesise information from multiple domains and deliver a more complete picture of tumour status,” shares Ma.
“This not only improves diagnostic accuracy but also allows the model to predict survival outcomes without additional training.”
The team further validated their approach in an independent cohort of glioblastoma patients.
The model’s predictions, particularly those related to tumour stability, significantly distinguished high-risk from low-risk groups (p=0.017), demonstrating prognostic value comparable to well-established biomarkers such as MGMT methylation status.
These findings highlight the potential of LLM-based integration to reduce diagnostic uncertainty and support more personalised treatment strategies in neuro-oncology.
The study, published in the KeAi journal Meta-Radiology, establishes a foundation for future research on multi-source integration in clinical oncology.
“Expanding the approach to include modalities such as MRI imaging and genomic profiles could further enhance predictive power and accelerate progress toward precision cancer care,” adds Ma.
Source: KeAi Communications Co., Ltd.
The World Cancer Declaration recognises that to make major reductions in premature deaths, innovative education and training opportunities for healthcare workers in all disciplines of cancer control need to improve significantly.
ecancer plays a critical part in improving access to education for medical professionals.
Every day we help doctors, nurses, patients and their advocates to further their knowledge and improve the quality of care. Please make a donation to support our ongoing work.
Thank you for your support.