Glioblastoma is a devastatingly effective brain cancer. Doctors can cut it out or blast it with radiation, but that only buys time. The cancer has an insidious ability to hide enough tumour cells in tissue around the tumour to allow it to return as deadly as ever.
Patients diagnosed with glioblastoma survive for an average of 15 months.
What’s needed is a better way of identifying those hidden cancer cells and predicting where the tumour might grow next.
Jennifer Munson believes she and her research team at the Fralin Biomedical Research Institute at VTC have developed a tool to do just that.
Their method, described this week in npj Biomedical Innovations, combines magnetic resonance imaging, Munson’s in-depth knowledge of how fluid moves through human tissues, and an algorithm Munson’s team developed to identify and predict where the cancer might reappear.
“If you can't find the tumour cells, you can't kill the tumour cells, whether that's by cutting them out, hitting them with radiation therapy, or getting drugs to them,” said Munson, professor and director of the FBRI Cancer Research Centre — Roanoke. “This is a method that now we believe can allow us to find those tumour cells.”
Currently, doctors plan surgeries to remove glioblastoma tumours based on radiological scans, but that only provides a view of the area just outside the cancer’s edge.
During surgery, fluorescent dyes highlight cancer cells, but the dyes don’t penetrate deeply and the cells have to be visible to the eye.
“Those methods are not going to see a cell that has migrated or invaded further into the tissue, which is something that we think we can do with this method,” said Munson, who also holds an appointment in Virginia Tech’s Department of Biomedical Engineering and Mechanics.
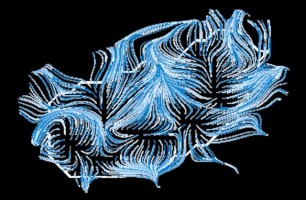
Munson’s research focuses primarily on interstitial fluid flow — the movement of fluid through the spaces between cells in tissues. The flow behaves differently in different diseases.
In studying glioblastoma, Munson’s lab found that faster flows predict where tumour cells are invading. More random motion of the fluid, or diffusion, however, correlates with less invasion by the cancer cells.
But a new metric Munson’s team developed proved to be the best predictor. The fluid flow around the tumour establishes pathways, like streams merging into rivers, which the cancer cells follow to migrate into the surrounding tissue.
“This could tell a surgeon where there's going to be a higher chance of there being more tumour cells, so they might be a little more aggressive, if it's safe to the patient to go after a more invasive region,” Munson said.
Munson’s findings underpin the work of a new spinoff company, Cairina, which aims to improve cancer treatment through a more personalised approach to surgery and cancer therapies. “Cairina is trying to take this to the next level,” Munson said.
“Our goal is to supply surgeons and radiation oncologists with probability maps or hotspot maps, where we would predict more cancer cell invasion to support more aggressive therapeutic application, and also to identify where there may be less invasion, to help spare tissue from unnecessary treatment.”
Article: Interstitial fluid transport dynamics predict glioblastoma invasion and progression
Source: Virginia Tech
Image credit: Jennifer Munson / Virginia Tech
The World Cancer Declaration recognises that to make major reductions in premature deaths, innovative education and training opportunities for healthcare workers in all disciplines of cancer control need to improve significantly.
ecancer plays a critical part in improving access to education for medical professionals.
Every day we help doctors, nurses, patients and their advocates to further their knowledge and improve the quality of care. Please make a donation to support our ongoing work.
Thank you for your support.