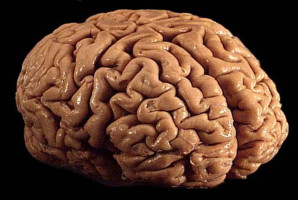
A new clinical guideline from the American Society for Radiation Oncology (ASTRO) focuses on the use of radiation therapy to treat adult patients with World Health Organisation (WHO) grade 4 diffuse gliomas, a category that includes some of the most common and most aggressive primary brain tumours.
The guideline, which replaces ASTRO’s 2016 guideline for glioblastoma, is published in Practical Radiation Oncology.
Glioblastomas, which were recharacterised under the WHO’s updated framework in 2021 as grade 4 adult-type diffuse gliomas, account for just under half of all malignant brain tumours in adults and are diagnosed in an estimated 10,000 Americans each year.
These tumours tend to grow quickly and infiltrate nearby brain tissue, and they carry a poor prognosis despite recent advances in radiation, surgical and systemic therapies that have improved median survival and quality of life for many patients.
Radiation therapy is a key component of treatment for diffuse gliomas because they rarely can be completely removed with surgery.
The 2021 WHO reclassification redefined the way gliomas are graded to incorporate newly discovered molecular markers, moving beyond histology alone to more precisely diagnose and treat these tumours.
ASTRO’s updated guideline reflects these changes, as well as the adoption of new, advanced imaging techniques and emerging treatments.
“As oncologists, high-grade gliomas are among the most challenging cancers we see, and radiation therapy plays a vital role in improving outcomes for these patients,” said Joseph A.Bovi, MD, chair of the guideline task force and a radiation oncologist at ThedaCare Regional Cancer Centre in Appleton, Wisc.
“This guideline brings together the best evidence across multiple disciplines to support coordinated care that includes surgery, radiation therapy, systemic therapies, alternating electric field therapy and supportive care."
“Our goal was to equip clinicians with a clear, robust framework for shared decision-making with their patients, while also highlighting areas where research is needed to move the field forward,” said Debra Nana Yeboa, MD, vice chair of the guideline task force and an associate professor of radiation oncology at the University of Texas MD Anderson Cancer Centre in Houston.
“Progress in personalised medicine, biomarker discovery, and advanced treatment techniques could help us change outcomes for patients, particularly those in underserved populations.”
The guideline’s evidence-based recommendations address multidisciplinary management of WHO grade 4 adult-type diffuse gliomas, including treatment indications and optimal radiation dosing, fractionation and techniques after initial biopsy/resection, as well as for reirradiation.
The guideline also includes visual algorithms for classification and management of this disease.
Key recommendations are as follows:
Fractionated radiation therapy (RT) is recommended for patients who have undergone biopsy or resection, based on several randomised controlled trials finding increased survival with RT compared to chemotherapy or supportive care alone. The guideline discusses optimal timing and fractionation schedules for adjuvant RT.
Temozolomide (TMZ) chemotherapy given concurrently with RT and following RT is also recommended after biopsy or resection. Alternating electric field therapy is conditionally recommended after RT for patients with tumours in the upper regions of the brain (i.e., supratentorial disease).
Recommendations outline suggested dose-fractionation regimens for RT guided by the patient’s age and functional status. Shorter radiation courses are conditionally recommended for elderly patients and those with indications of frailty. For patients with severe frailty, who have notably increased risk of complications from intensive treatments, supportive care in lieu of chemoradiation is conditionally recommended following a multidisciplinary, patient-centred discussion. Supportive care, including palliative services, is also discussed in the context of helping patients manage symptoms during and after treatment. The guideline also discusses recommended treatment techniques and target volumes and notes the importance of daily image guidance during RT.
Reirradiation for WHO grade 4 diffuse glioma recurrence is conditionally recommended for selected adult patients with good functional status, following a multidisciplinary, patient-centred discussion. The guideline also reviews indications and techniques for reirradiation including diagnostic and treatment considerations, as well as systemic therapy in the reirradiation setting.
The task force also reviewed the literature on health disparities and adult high-grade glioma, calling to attention the need for more studies that examine barriers to access and the need to increase clinical trial enrollment for underserved populations.
About the Guideline
“Radiation Therapy for WHO Grade 4 Adult-Type Diffuse Glioma: An ASTRO Clinical Practice Guideline” was based on a systematic review of articles published from March 2014 through December 2023.
The multidisciplinary guideline task force included radiation, medical and neurosurgical oncologists; a neuropathologist; a radiation oncology resident; a medical physicist and a patient representative.
The guideline was developed in collaboration with the American Association of Neurological Surgeons/College of Neurological Surgeons, the American Association of Neuropathologists, the American Society of Clinical Oncology and the Society for Neuro-Oncology.
It is endorsed by the European Society for Radiotherapy and Oncology and the Royal Australian and New Zealand College of Radiologists.
ASTRO's clinical guidelines are intended as tools to promote appropriately individualised, shared decision-making between physicians and patients.
None should be construed as strict or superseding the appropriately informed and considered judgments of individual physicians and patients.
The World Cancer Declaration recognises that to make major reductions in premature deaths, innovative education and training opportunities for healthcare workers in all disciplines of cancer control need to improve significantly.
ecancer plays a critical part in improving access to education for medical professionals.
Every day we help doctors, nurses, patients and their advocates to further their knowledge and improve the quality of care. Please make a donation to support our ongoing work.
Thank you for your support.