Results from the Phase 3, randomised, placebo-controlled VERIFY study evaluating rusfertide in patients with polycythemia vera (PV) were presented as a late-breaking oral presentation at the 61st American Society of Clinical Oncology (ASCO) Annual Meeting Plenary Session.
The study was found to have met the primary and all key secondary endpoints.
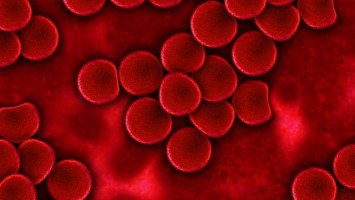
PV is characterized by overproduction of red blood cells (erythrocytosis), which may increase blood viscosity, or thickness, potentially resulting in life threatening thrombotic events such as stroke, deep vein thrombosis and pulmonary embolism. People with PV can experience burdensome symptoms, including severe fatigue, difficulty in concentrating, night sweats and pruritus, which may negatively impact their daily functioning and quality of life. Haematocrit is the ratio of red blood cells to total amount of blood in the body. Achieving and maintaining controlled haematocrit levels of <45% is the primary treatment goal in PV to prevent thrombotic events and alleviate symptoms, but many patients still experience uncontrolled haematocrit levels with current standard of care treatments.
Rusfertide, an investigational, first-in-class hepcidin mimetic peptide therapeutic, is under evaluation in the Phase 3 VERIFY study for its potential to regulate iron homeostasis and red blood cell production to control haematocrit levels in patients with PV.
In the study, patients dependent on frequent phlebotomy, with or without treatment with cytoreductive therapy, were randomised to receive once-weekly rusfertide or placebo, as an add-on to current standard of care treatment.
“PV poses significant challenges for patients, including debilitating symptoms and the risk of serious thrombotic events, and haematocrit control is crucial to improving patient outcomes. The VERIFY study demonstrated that treatment with rusfertide controls haematocrit levels in phlebotomy-dependent patients, including patients receiving cytoreductive therapies,” said Dr. Andrew T. Kuykendall, M.D., VERIFY Lead Investigator and Associate Member in the Department of Hematology at Moffitt Cancer Center. “These results suggest rusfertide has the potential to become part of the standard of care treatment for patients with PV.”
The study met its primary endpoint, which was the proportion of patients achieving a clinical response, defined as the absence of phlebotomy eligibility during study Weeks 20-32. Study results demonstrated 76.9% of patients treated with rusfertide plus current standard of care achieved a clinical response, compared to 32.9% in the placebo plus current standard of care group (p<0.0001).
The response observed in the rusfertide arm was consistent across subgroups, regardless of risk status or type of concurrent cytoreductive therapy. In addition, all key secondary endpoints met statistical significance in favour of the rusfertide arm compared to the placebo arm in the VERIFY study.
The mean number of phlebotomies was 0.5 phlebotomies per patient for those treated with rusfertide plus current standard of care compared to 1.8 phlebotomies per patient for those treated with placebo plus current standard of care during Weeks 0-32 (p<0.0001).
Only 27% of patients treated with rusfertide plus current standard of care required phlebotomy between Weeks 0-32, compared to 78% of patients who received placebo plus current standard of care.
The mean number of phlebotomies during Weeks 0-32 in the rusfertide arm was reduced across subgroups, including risk status and use of concurrent cytoreductive therapy, versus the placebo arm.
62.6% of patients treated with rusfertide plus current standard of care maintained haematocrit levels below 45% versus 14.4% treated with placebo plus current standard of care (p<0.0001).
Rusfertide also showed statistically significant improvements in mean change from baseline to Week 32 in PROMIS Fatigue (p<0.03) and the MFSAF Total Symptom Score3 (p<0.03). Rusfertide is the first investigational therapy to prospectively demonstrate a statistically significant improvement in these patient-reported outcomes (PROs) of fatigue and symptom burden in patients with PV.
Rusfertide was generally well tolerated. The majority of adverse events were low grade and non-serious and no serious adverse events considered related to rusfertide were reported. There was no evidence of increased risk of cancer in patients treated with rusfertide plus current standard of care compared to patients treated with placebo plus current standard of care at the time of the primary analysis. Cancer events were reported in one patient in the rusfertide arm (0.7%) and in seven patients in the placebo arm (4.8%). The most common treatment-emergent adverse events were localized injection site reactions (55.9%), anaemia (15.9%) and fatigue (15.2%).1
Rusfertide has received Orphan Drug designation and Fast Track designation from the U.S. Food & Drug Administration.
Source: Takeda
We are an independent charity and are not backed by a large company or society. We raise every penny ourselves to improve the standards of cancer care through education. You can help us continue our work to address inequalities in cancer care by making a donation.
Any donation, however small, contributes directly towards the costs of creating and sharing free oncology education.
Together we can get better outcomes for patients by tackling global inequalities in access to the results of cancer research.
Thank you for your support.