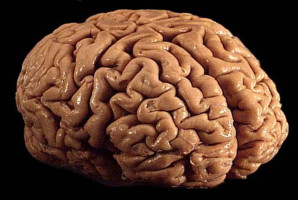
Glioblastoma multiforme is an aggressive brain tumour that mainly affects adults.
Approximately 30,000 people in the U.S. are diagnosed with GBM every year and patients have a 5-year survival rate of 7%.
Current treatments include surgery, radiation therapy and chemotherapy with temozolomide.
Unfortunately, none of these methods can cure GBM.
In a study, University of Michigan researchers have created nanodiscs that can target cholesterol levels in GBM, starving the cancer cells and increasing survival rates of the treated mice.
“Treatment options for GBM have their limitations,” said Maria Castro, professor of neurosurgery and a member of the Rogel Cancer Centre.
“Although surgery can help improve survival, surgeons often have to remove the normal tissue that surrounds the tumour to prevent it from spreading. On the other hand, using drugs to target the cancer is also challenging because GBM cells are heterogeneous. If you try and target a particular pathway, the cancer cells can use other pathways and repopulate the tumour.”
Additionally, anti-cancer drugs cannot easily cross the blood-brain barrier, which protects the brain from substances in the blood, according to Anna Schwendeman, professor of pharmaceutical sciences.
Previous studies have shown that GBM tumours require cholesterol to proliferate.
However, they are unable to make enough of it and instead import cholesterol from other cells.
The team created specific nanodiscs and injected them into mouse models for GBM.
“Our goal was to provide surgeons with the option to inject these particles into the tumour cavity after they have removed the tumour mass,” said Troy Halseth, former graduate student in the Schwendeman and co-first author on the study.
“It is important to focus on local delivery because chemotherapy drugs are toxic and can cause several side effects.”
The nanodiscs were synthesised to deliver Liver-X-Receptor agonists to the cancer cells.
These molecules increase the number of pumps that can export cholesterol out of the tumour cells, resulting in their death.
When used in combination with radiation therapy, more than 60% of the mice survived when compared to the mice that only received radiation.
“We included radiation because it is the standard procedure of care for GBM patients. Therefore, any new therapy must be given in addition to radiation,” said Anzar Mujeeb, postdoctoral fellow in the Castro lab and co-first author on the study.
The combined treatment was able to preserve normal brain structure and there were no adverse side effects.
The nanoparticles also had CpG oligonucleotides on their surface, which activate the body’s immune system.
As a result, immune cells not only attack the tumour, but also retain the memory and are able to attack any future tumours.
“The main cause of death in glioma patients is not the primary cancer, which is usually removed efficiently by surgeons. Instead, it is when the tumour comes back,” Castro said.
“We wanted to address that problem as well.”
The researchers discovered that in addition to prolonging the survival rates, the nanodiscs also elicited an immunological memory and 68% of the surviving mice eliminated the second tumour that was introduced into their bodies.
The team is now working on scaling up the synthesis of these particles and planning a clinical trial.
“This study would not have been possible without the interdisciplinary collaboration between U-M cancer biologists and drug delivery experts from the School of Pharmacy,” Schwendeman said.
Additional authors: Lisha Liu, Kaushik Banerjee, Nigel Lang, Todd Hollon, Minzhi Yu, Mark Vander Roest, Ling Mei, Hongliang He and Maya Sheth.
Funding/disclosures: The work was supported by National Institutes of Health and National Institute of Neurological Disorders and Stroke grants R37- NS094804, R01-NS105556, R01-NS122536, R01-NS124167 and R21-NS123879-01 and Rogel Cancer Centre Scholar Award.
This work has also been supported by the Biosciences Initiative in Brain Cancer Technologies, U-M Department of Neurosurgery, Paediatric Brain Tumour Foundation and Ian's Friends Foundation.
Halseth was supported by the Predoctoral Fellowship in Drug Discovery from the PhRMA Foundation.
Yu was supported by American Heart Association Postdoctoral Fellowship (24POST1196020).
The World Cancer Declaration recognises that to make major reductions in premature deaths, innovative education and training opportunities for healthcare workers in all disciplines of cancer control need to improve significantly.
ecancer plays a critical part in improving access to education for medical professionals.
Every day we help doctors, nurses, patients and their advocates to further their knowledge and improve the quality of care. Please make a donation to support our ongoing work.
Thank you for your support.