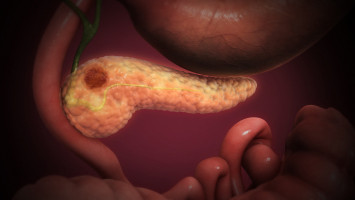
Researchers at OU Health Stephenson Cancer Center at the University of Oklahoma Health Sciences have embarked on a revolutionary new research study that could improve the detection of a deadly disease — pancreatic cancer — and give patients a chance to live longer, healthier lives.
The research focuses on an innovative combination of imaging techniques: a newly created contrast agent that recognises pancreatic cancer cells, paired with Multispectral Optoacoustic Tomography, or MSOT.
Together, the approach can detect pancreatic cancer cells the width of an eyelash — approximately 10 times more magnitude than what is currently possible.
The research is led by Lacey McNally, Ph.D., and Ajay Jain, M.D., who are professors of surgery at the OU College of Medicine.
They received a $3 million grant from the National Cancer Institute of the National Institutes of Health for this project, which is believed to be among the first of its kind in the world.
“Pancreatic cancer is one of the hardest cancers to cure because it is difficult to detect cancer cells at the microscopic level,” Jain said.
“Because there are usually no early symptoms of pancreatic cancer, it is typically not diagnosed until after it has spread, and outcomes are very poor — about a 9% overall chance of survival.
Surgery and chemotherapy offer the patients the best chance, but for surgery to work, we have to remove all the cancer, and that is difficult to do.”
The new imaging approach aims to improve the detection of pancreatic cancer cells at the microscopic level, or about 200 microns, about as thin as an eyelash.
Current imaging options like the CT scan only detect cancer when it grows larger, about a centimeter in size.
The promise of the new imaging approach is in the combined strength of its two elements.
In the laboratory, McNally devised a contrast agent unique to pancreatic cancer cells.
When the agent is delivered via an IV, it can differentiate pancreatic cancer cells from other cells because the environment of pancreatic cancer is acidic.
When the contrast agent encounters that acidity, its dye essentially “turns on.”
The other component, the MSOT device, works in concert with the contrast agent.
The MSOT delivers infrared light into the body, which stimulates the dye of the contrast agent.
That stimulation creates sound waves, which the MSOT device picks up and converts into colours.
The result is an image so detailed that it captures cancer cells that otherwise would evade detection.
“This is a hybrid approach that accomplishes what a CT cannot,” McNally said.
“Pancreatic cancer often creates tentacles that spread out beyond the primary tumour. Currently, there is no way for the surgeon to know where they are. But if the surgery team can use this MSOT approach in the operating room, it can tell them in real time where the cancer has metastasized so they can remove it.”
That capability would be a game-changer for pancreatic cancer surgeons.
Pancreatic cancer disproportionately affects people 60 and older, who face greater risks from a major operation than younger patients do and usually cannot withstand a second surgery.
“The first questions patients ask me are, ‘Will the surgery be worth it? What are the chances that you’ll get it all?’ This approach, at a very microscopic level, appears able to inform us whether we are getting all the cancer,” Jain said.
The new imaging technique could also help surgeons plan the surgical approach they want to take.
If the MSOT device reveals, for example, that cancer has invaded the two critical blood vessels that hug the head of the pancreas, surgeons would conduct the procedure differently than if they didn’t know.
If chemotherapy is given before surgery, the imaging could tell whether cancerous cells on the blood vessels are dead or if microscopic cancer is still present.
Ultimately, the new imaging approach could be used as a screening tool in patients who face a high risk of pancreatic cancer, such as those who have a family history or have a genetic predisposition.
“Early detection of pancreatic cancer offers the best chance of a cure,” Jain said. “If we could detect the cancer at an early, microscopic stage, it could be curable.”
The grant's funding will allow McNally and Jain to continue testing the imaging technique.
McNally is an international leader for her research expertise in using the MSOT device with contrast agents she has developed for various cancers.
She is testing the imaging approach in several other clinical trials at OU Health Sciences, including a recently completed study in breast cancer.
While MSOT technology is not new, it is novel in medicine, and funding agencies like the NIH are increasingly supporting studies in the field.
McNally and Jain’s grant scored in the first percentile out of approximately 55,000 grants submitted last year to the National Cancer Institute, which points to the strength of the research.
“This type of research collaboration between a translational scientist and a surgeon is extremely unusual,” McNally said.
“We have the opportunity to improve a surgical technique. The scientific and medical communities have made great strides in treating some types of cancer, but pancreatic cancer patients have the poorest survival. The outcome of this research could fundamentally change people’s lives.”
The University of Oklahoma and Georgia State University jointly own pending patent applications on contrast agents and using the MSOT device with contrast agents.
Source: University of Oklahoma