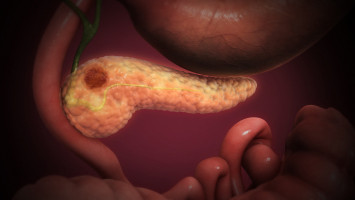
Pancreatic cancer is one of the most difficult cancers to treat, being highly resistant to chemotherapy.
However, there are no effective alternative therapies to chemotherapy, so chemo remains the best available treatment.
Although there are fewer than roughly 60,000 new cases of pancreatic cancer diagnosed annually in the U.S., about 95 percent of people with it die from it, mainly because it often goes undetected in early stages.
Approved multi-agent chemotherapy regimens offer a marginal advance over single-agent treatments, and resistance to these “cocktails” virtually always develops.
Multi-agent chemo offers a median survival benefit of roughly four months over a single-agent.
Overall, the median survival of patients with metastatic pancreatic cancer in the modern era is just eight to 11 months, and the five-year survival rate is around 3 percent.
Physicians hope that adjuncts, or added chemical formulations, may be discovered in the future to improve the effectiveness of chemotherapy against this disease and improve survival outcomes.
In a new study, published June 28 by the prestigious science journal Nature Communications, researchers from University Hospitals Seidman Cancer Center and the Case Comprehensive Cancer Center report that a hyperglycaemic state – that is, one where the blood glucose level is raised – made pancreatic cancer more sensitive to chemotherapy in a mouse model.
(Pancreatic cancer is more formally known as Pancreatic Ductal Adenocarcinoma and shortened as PDAC).
Results were replicated in cell culture and a cohort of patients with metastatic PDAC.
These findings present a potentially new method of making chemotherapy more effective against pancreatic cancer, according to the paper’s senior author Jordan Winter, MD, Director Surgical Services, University Hospitals Seidman Cancer Center, John and Peggy Garson Family Endowed Chair in Pancreatic Cancer research and Jerome A. and Joy Weinberger Family Master Clinician in Surgical Oncology.
“Sensitization of tumours to chemotherapy using forced hyperglycaemia offers a completely novel therapeutic strategy.
Our findings reveal an approach that would have a relatively low-cost and could be easily tested in patients with pancreatic cancer,” said Dr. Winter.
Over the past three decades, pancreatic cancer researchers have yet to find new effective targeted therapies.
However, if relatively simple interventions can be administered that can greatly enhance the effect of conventional drugs, then patients stand to benefit.
Importantly, this advance would potentially bypass the usual cost and time required to develop new therapeutics.
This could save over a decade of time and more than $1 billion, based on drug development data.
In the study, the researchers validated a prior clinical study by the same authors that showed patients with localised pancreatic cancer and elevated glucose levels were more responsive to chemotherapy.
For the current study, the researchers examined the impact of glycaemic status on another group of patients treated for metastatic pancreatic cancer.
About 33 percent of the patients had elevated glucose levels (at least one glucose reading above 200 mg/dL).
There were no appreciated demographic differences between normal (99 mg/dL or lower) and high glucose patients.
A greater proportion of patients in the high glucose group had a documented diagnosis of diabetes.
The median overall survival among all patients who completed at least two cycles of chemotherapy was approximately 9.8 months in all the patients, on par with historical clinical trial data.
Further analysis showed, however, that patients in the high glucose level group had a nearly 40% lower risk of dying, despite a higher level of a cancer antigen (CA19-9, which is a measure of disease burden), as compared to patients in the normal glucose group.
“Notably, no associated survival difference was observed based on glucose levels in an independent cohort of metastatic patients who did not receive treatment, suggesting that the interaction with glycaemic status may be present only for patients who receive chemotherapy,” said lead author Ali Vaziri-Gohar, PhD, of the Case Comprehensive Cancer Center at Case Western Reserve University at the time of the study and now with the Stritch School of Medicine, Loyola University Chicago,
Paired with prior cell culture and clinical data, these clinical data indicated that a high-glucose state could sensitise PDAC to conventional chemotherapy.
The researchers followed up on these findings with a series of well-controlled studies in various mouse PDAC models of hyperglycaemia.
First, they induced hyperglycaemia pharmacologically with a drug called streptozotocin (STZ).
In another group of experiments, they induced hyperglycaemia through diet, allowing mice to drink highly sweetened water at will.
In experiments with grafted PDAC tumours on hyperglycaemic mice, the researchers found greater sensitivity to single-agent chemotherapy in the two independent models of mice with hyperglycaemia.
As observed previously with patients in the absence of chemotherapy, no significant differences in growth rates were observed with hyperglycaemia compared to mice with normal blood sugar levels in the absence of chemotherapy exposure.
The researchers also tested a multiple-agent chemotherapy to replicate what a patient might receive today and validated that hyperglycaemia alters the metabolic state within tumours to sensitise it to treatment.
“We show that the effectiveness of diverse chemotherapies was markedly improved under high glucose conditions, as compared to low glucose conditions. In some instances, the mice appeared to be cured of their cancer, while mice receiving the same chemotherapy under normal glycaemic conditions had relatively little benefit” said Dr. Winter.
"How can this observation be translated to patients? In the clinical setting, tumours can be theoretically ‘primed’ for chemotherapy by inducing a forced hyperglycaemic state, just as we did in mice. In theory, glucose levels can even be modified more precisely through intravenous dextrose infusions (combined with rigorous inpatient glucose monitoring) at the time of chemotherapy administration. The next step is to implement a clinical trial."
Dr. Winter notes that “our patients need better treatment options urgently. Therefore, we are already getting to work designing a trial to treat patients safely with intentionally elevated blood sugars, and will determine if this strategy can improve patient outcomes.”