
By Dr Ibtihal Fadhil - Founder and Chair of the Eastern Mediterranean NCD Alliance, Former, Regional Adviser NCD, WHO/EMRO and Member of the MENA HPV Coalition
World HPV Awareness Day, which takes place on March 4, offers a chance for individuals from all over the world to get together to spread awareness of the value of the HPV vaccine, prevention, and early detection of cervical cancer. We can significantly advance the elimination of cervical cancer in many countries by boosting knowledge and access to HPV vaccinations.
Cervical cancer is a preventable disease caused by the human papillomavirus (HPV). Cervical cancer is the fourth most common cancer amongst women causing over 300,000 deaths worldwide in 20201. Cervical cancer-related deaths of women of working age have terrible socioeconomic repercussions that have a significant negative impact on families and communities.
Yet, HPV is not just a significant contributor to cancer in women; it also has an impact on men. Oropharyngeal and oral cavity cancers, as well as penile cancer in men, are cancers linked to HPV that can affect both genders2.
Fortunately, early detection and prevention are effective approaches to lower the occurrence of cervical cancer. Vaccination is one of the best ways to prevent cervical cancer and HPV infection. Cervical cancer prevalence can be decreased with vaccination, eventually leading to its eradication. Cervical cancer risk has been demonstrated to be reduced by up to 90% by vaccination against HPV infection. It is crucial to remember that the HPV vaccine is reliable, safe, and does not raise the chance of developing cancer.
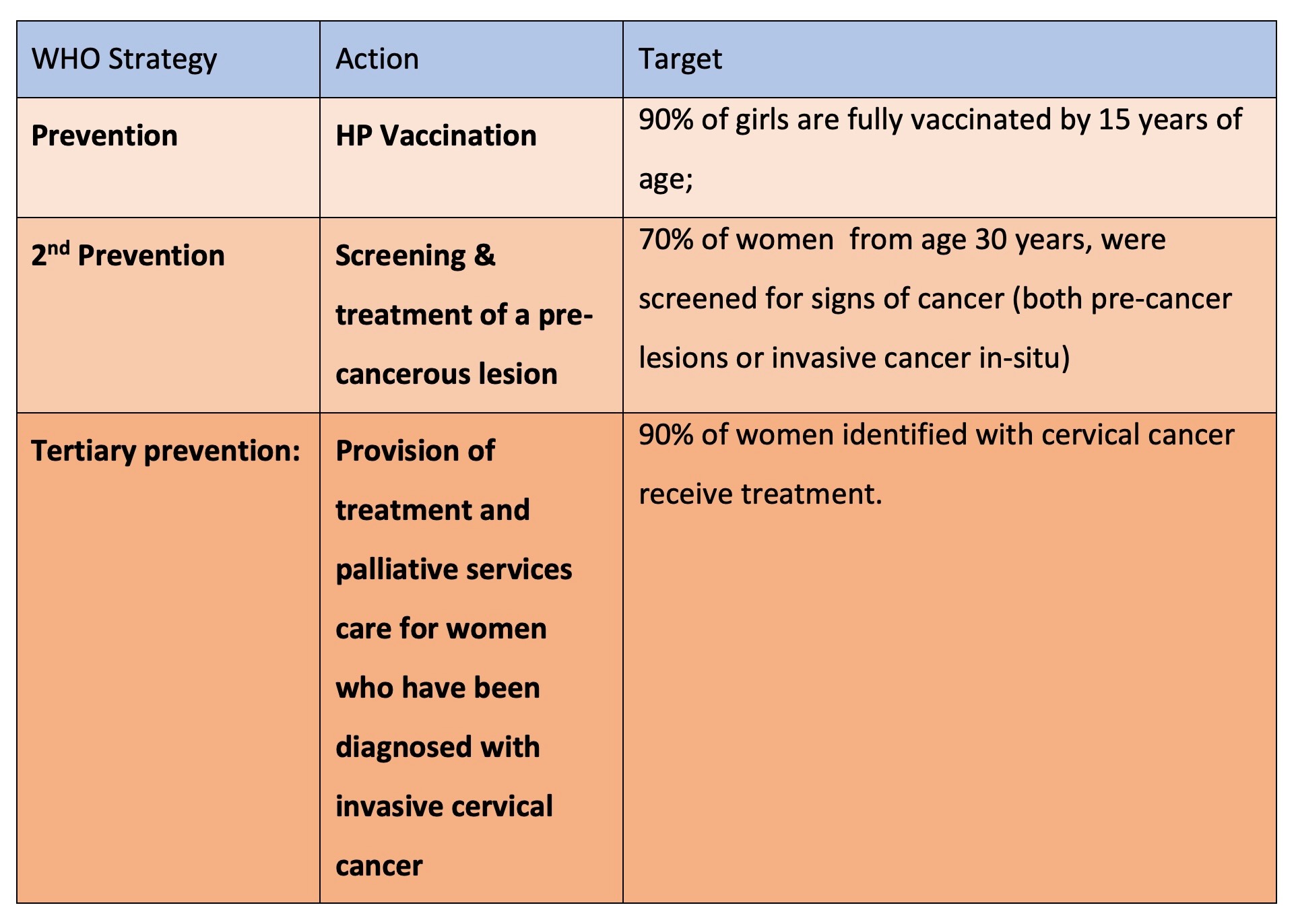
The World Health Organization (WHO) has set a goal to eliminate cervical cancer as a public health problem by 2030. To achieve this goal, it is essential that all countries increase efforts through proven effective interventions across three interrelated streams of work with a set of targets Known as the 90-70-90 target to be achieved by 20303.
The elimination of cervical cancer has been incorporated into the 2030 Sustainable Development Goals, the Global Strategy for Women, Children, and Adolescents' Health (2016-2030), the Global Health Sector Strategy on HIV, Hepatitis, and STIs (2016-2021), Health Systems Strengthening for Social Protection, and Universal Health Coverage in order to promote multi-partner and multi-stakeholder collaborations.
Regional Perspective
According to the WHO, cervical cancer is the sixth most prevalent malignancy in women in the WHO's Eastern Mediterranean Region, making it a significant public health issue in the region. In 2020 an estimated 89 800 women are diagnosed with cervical cancer and more than 47 500 women died from this preventable disease.4
In the region, different countries have different rates of cervical cancer. Age-standardised incidence rates are much higher in four countries (Somalia, Morocco, Djibouti, and Libya) than the goal incidence rate for elimination, which is 4 cases per 100,000. All of these rates are greater than 10 per 100,000. Afghanistan, Lebanon, Oman, Pakistan, Sudan, and the UAE were among the intermediate-level nations, with rates between the 4 per 100,000 thresholds and less than 10 per 100,000. While low rates (age-standardised rates of 4 per 100,000 or less) were reported in Bahrain, Egypt, the Gaza Strip, the West Bank, the Islamic Republic of Iran, Iraq, Jordan, Kuwait, Qatar, Saudi Arabia, Tunisia, and Yemen.
Although the majority of the countries in the region have very low rates of cervical cancer, there is a chance of an increase that needs to be considered. The region is more likely to be exposed to a wide range of risk factors for both communicable and non-communicable diseases due to the effects of globalisation and the growth in domestic and international travel. Most of the Gulf countries have experienced over the past thirty years substantial increases in the numbers of non-nationals that now reside in these countries. Other countries face the influx of tourists particularly from Europe where risk factors for many diseases are at times higher than in EM region countries.
In response to this alarming trend, the World Health Organization (WHO) launched a Regional Cervical Cancer Elimination Strategy for the Eastern Mediterranean Region in 20205. This strategy aims to reduce the burden of cervical cancer in the region by increasing access to prevention, diagnosis, and treatment services.
The WHO also published a report on the profile of cancer in the EMR, which highlighted the need for improved cancer surveillance and control programmes in the region.6 The report identified several risk factors for cervical cancer, such as early marriage, multiple sexual partners, and lack of access to screening and treatment service
HPV vaccine hesitancy in the region
Available data indicate that only five countries out of 22 EMR countries provided HPV immunisation in their national immunisation programmes (Morocco, Qatar, KSA, UAE, and Libya)7. HPV vaccination is linked to uncertainty and false information in the region.
Additionally, nations with an incidence rate currently below the global targets expressed reluctance to adopt the HPV vaccine.
Although cervical cancer rates in some countries are low, it is still advisable for those countries to use the HPV vaccine.
The World Health Organization (WHO) states that the foundation for lowering every country's incidence rate of cervical cancer to the agreed elimination level is immunising girls against cancer-causing varieties of human papillomavirus (HPV) before the age of 15. For the prevention of HPV serotypes 16 and 18, which are responsible for 70% of cervical cancer, the HPV vaccine is very effective. The widespread administration of the HPV vaccine significantly lowers the number of women who will develop cervical cancer according to a Swedish study8. Consequently, it is crucial to prevent cervical cancer even in countries with low rates.
To reduce the burden of cervical cancer in the EMR, it is essential to address these risk factors and improve access to HPV vaccination rates. Innovative prevention and integrative screening and management programmes are urgently needed to mitigate the increasing rate in the region. Further investigation into the epidemiology of HPV in the region is necessary as is raising public awareness of the value of HPV vaccination in this region. There is also a need for a tailored approach that takes into account country resources and context. The need to integrate cervical cancer interventions as part of a UHC benefit package.
For further information watch an interview with Dr Fadhil here.
References: