A single drug compound simultaneously attacks hard-to-treat prostate cancer on several fronts, according to a new study in mice and human cells.
It triggers immune cells to attack, helps the immune cells penetrate the tumour, and cuts off the tumours' ability to burn testosterone as fuel, according to new research from Washington University School of Medicine in St Louis.
The drug may offer a promising new strategy for treating patients whose tumours don’t respond to standard therapy.
The study appears online in the journal Nature Communications.
Prostate cancer is notorious for eventually developing resistance to standard treatments that block or reduce testosterone, which fuels growth of these tumours.
And like many solid tumours, prostate cancer also has proven stubbornly resistant to newer immunotherapies, which are intended to take the brakes off the immune system’s T cells to get them fighting cancerous invaders.
Immunotherapies — most commonly, immune checkpoint inhibitors — can be extremely effective but only in certain cancers, such as melanoma.
“We need to develop better therapies for prostate cancer patients, because most of these tumours develop resistance to hormone-based therapies doctors rely on to treat these cancers,” said senior author Nupam P Mahajan, PhD, a professor of surgery. “Immunotherapy is the newest and most promising type of therapeutic for cancer right now, but even so, immune checkpoint inhibitors have failed to do much against most solid tumours, including prostate cancer. This study was surprising because we found that this drug activates anti-cancer T cells in a novel way, and it also increases the T cells’ ability to penetrate the tumour. This could lead to a more effective strategy for patients whose cancers are hard to treat.”
The drug, called (R)-9b, is a small molecule that blocks an oncogene, a gene that drives cancer.
The researchers initially attributed the drug’s success in mouse studies to its ability to reduce or eliminate androgen receptors in the prostate cancer cells.
These receptors bind to testosterone and use the hormone to fuel tumour growth.
The drug’s ability to eliminate the androgen receptor differs from standard drugs that reduce the amount of testosterone in the body, and other drugs that block the androgen receptor’s function as a transcription regulator.
But because the new drug was so effective, Mahajan and his colleagues suspected something more was going on.
The drug blocks a gene called ACK1.
The researchers developed a strain of mice that totally lacked this gene in order to study what happens when it’s missing.
At first, the researchers were baffled by these mice.
Mice missing an entire gene often have obvious problems.
But these mice seemed fine.
And when the researchers looked for tumour growth, they found very little.
It was difficult to model cancer in these animals.
“In most of these mice, when we introduced cancer cells as we typically do, there was no trace of a tumour,” said Mahajan, also a research member of Siteman Cancer Centre at Barnes-Jewish Hospital and Washington University School of Medicine. “In the few that did develop tumours, the tumours were small compared to those of wild-type mice. This was the first clue that something important was happening in mice missing this gene. We found that they were able to mount a robust immune response against the cancer cells.”
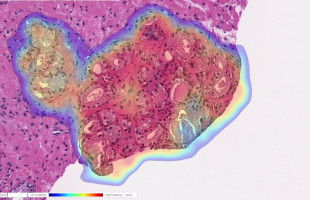
When different mice — mice with this gene — were implanted with human prostate tumours and given the drug that blocks this gene, it had the same effect: taking the brakes off the immune system and producing increased levels of certain types of T cells known to attack cancer.
The drug also increased signalling molecules that allow the T cells to penetrate the tumour and kill cancer cells more effectively.
The tumours in these (R)-9b treated mice were much smaller than those of mice in control groups.
Given the drug’s success in tumour penetration, the researchers investigated whether adding immune checkpoint inhibitors to treatment with the drug would be even more effective, taking the brakes off T cells in more than one way at the same time — but there was no such improvement.
“Surprisingly, we found that the immune checkpoint inhibitor is activating ACK1, the very pathway we are shutting down with this drug compound,” Mahajan said. “It’s possible immune checkpoint inhibitors don’t work well in these tumours because they are turning on ACK1, which suppresses the immune response. Similar to prostate cancer, the ACK1 pathway activation also could be employed by other cancers that do not respond to checkpoint inhibitors. However, these cancers could respond to (R)-9b, so we would like to investigate this drug in other solid tumours as well.”
Mahajan said the drug spurs multiple responses because of the nature of the gene it blocks.
Many genes have several roles in the body, and ACK1’s roles in expression of the androgen receptor and in reigning in the immune system make it an appealing target for cancer therapy, especially against solid tumours with a hormonal growth component, such as prostate and breast cancers.
Mahajan has worked with Washington University’s Office of Technology Management/Tech Transfer to file patents on the use of this drug in cancer treatment.
His team is gathering data to apply for permission from the Food and Drug Administration to test the drug in a clinical trial for patients with prostate cancer.
Source: Washington University School of Medicine in St Louis
The World Cancer Declaration recognises that to make major reductions in premature deaths, innovative education and training opportunities for healthcare workers in all disciplines of cancer control need to improve significantly.
ecancer plays a critical part in improving access to education for medical professionals.
Every day we help doctors, nurses, patients and their advocates to further their knowledge and improve the quality of care. Please make a donation to support our ongoing work.
Thank you for your support.