Transfusion-dependent β-thalassemia (TDT) and sickle cell disease (SCD) are both caused by mutations in the haemoglobin β subunit gene that result either in markedly reduced/absent production of β chains of haemoglobin or abnormal haemoglobin polymerization upon deoxygenation.
Recently approved therapies such as luspatercept and crizanlizumab improve disease symptoms, but are not curative.
While allogeneic bone marrow transplantation can cure TDT and SCD, only a limited proportion of eligible patients can locate a compatible donor.
Studies have shown that improving levels of fetal haemoglobin (HbF) is associated with improved outcomes in patients with TDT and SCD.
Other studies have identified single-nucleotide polymorphisms (SNPs) in the BCL11A locus that are linked to increased expression of HbF and subsequently less severe disease.
Exagamglogene autotemcel (exa-cel), formerly known as CTX001 is an investigational cell therapy that uses CRISPR-Cas9 to edit the BCL11A locus in autologous haematopoietic stem and progenitor cells (HSPCs) and reactivate HbF production.
Previous studies with exa-cel showed impressive results in which a single dose of CTX001TM was sufficient to eliminate red blood cell (RBC) transfusions in TDT and vaso occlusive crises (VOCs) in SCD.
The CLIMB THAL-111 and CLIMB SCD-121 studies aimed to evaluate the efficacy and safety of exa-cel in 44 patients with TDT and 31 patients with SCD.
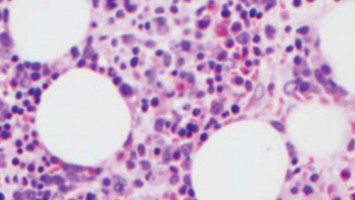
Myeloablation was performed using busulfan followed by exa-cel infusion containing BCL11A-edited HSPCs.
The patients were then followed up for an average of 12.3 and 9.6 months for TDT and SCD, respectively.
After the exa-cel infusion, RBC transfusions were eliminated in over 95% of patients with TDT and the two patients that still required transfusions were able to reduce the transfusion requirement by 75% and 89%.
Similarly, 31 patients with SCD no longer experienced severe VOCs.
HbF and total Hb levels showed clinically meaningful increases in both disease groups and were maintained throughout the follow-up period with stable proportions of edited BCL11A alleles in bone marrow HSPCs and peripheral blood mononuclear cells.
No patients with SCD and two patients with TDT exhibited serious adverse events related to exa-cel, although both SAEs resolved over time.
No deaths, discontinuations, or malignancies were reported.
In conclusion, a single CTX001TM infusion shows the remarkable ability to eliminate transfusions in patients with TDT and VOCs in patients with SCD, with stable increases in HbF and total Hb over time.
The consistent expression of edited BCLA11A alleles over 1 year indicated successful long-term editing of HSPCs and is the basis of a durable response.
Therefore, exa-cel represents a potentially transformative treatment for TDT and SCD.
Source: EHA
Watch the press conference on the study here
The World Cancer Declaration recognises that to make major reductions in premature deaths, innovative education and training opportunities for healthcare workers in all disciplines of cancer control need to improve significantly.
ecancer plays a critical part in improving access to education for medical professionals.
Every day we help doctors, nurses, patients and their advocates to further their knowledge and improve the quality of care. Please make a donation to support our ongoing work.
Thank you for your support.