New research from Roswell Park Comprehensive Cancer Center has uncovered genetic factors other than human leukocyte antigen (HLA) compatibility that significantly contribute to outcomes following blood and marrow transplant (BMT) in cancer patients. This study, published in the journal EClinicalMedicine, a Lancet open access journal, could lead to major changes in the way blood and marrow donors and recipients are matched as well as the development of new therapies to prevent transplant-related complications.
A team of investigators led by Theresa Hahn, PhD, Professor of Oncology in the Department of Cancer Prevention and Control at Roswell Park, that included collaborators from The Ohio State University, scanned the DNA of 2,887 cancer patients who underwent BMT between 2000 and 2011 for the treatment of acute myeloid leukaemia, myelodysplastic syndrome or acute lymphoblastic leukaemia, along with the DNA of their healthy HLA-matched unrelated donors.
“This study provides the first evidence that common genetic variation other than HLA compatibility significantly impacts survival following blood and marrow transplant, suggesting that there are important genetic variants other than HLA type to consider when matching unrelated donors and recipients,” says Dr. Hahn. “These findings could change the way in which unrelated donors and recipients are matched for BMT, and they could also help to guide posttransplant treatment strategies, providing more personalised treatment tailored to the individual patient’s unique genome, paving the way towards individualized risk prediction and prognosis to improve the success of BMT therapy for cancer.”
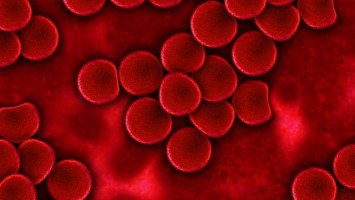
Allogeneic BMT, or the infusion of blood or marrow from a healthy donor to a recipient, is a curative treatment option for a variety of cancers, including leukaemia, myelodysplasia and lymphoma. To increase the odds of success, donors and recipients are matched according to HLA type, which increases the chance that the transplant will be successful and reduces the risk of potentially fatal transplant-related complications, like graft-versus-host disease. However, despite closely matching donors and recipients according to their HLA type, too many patients die within 1 year of BMT due to disease or complications related to the transplant itself, indicating that critical factors other than HLA type contribute to the success of BMT cancer therapy.
The team looked for genes outside of the HLA region that might be associated with BMT outcome. Using this genome-wide association approach, the investigators found that specific genes in donors and recipients, as well as specific combinations of donor and patient genes other than HLA genes, had a significant effect on the outcome of BMT for various types of cancer.
For example, in recipients, MBNL1, a gene related to leukaemia that is expressed in most blood and marrow cells, was associated with an increased risk of death in the first year after BMT, as was PILRB, a gene associated with immune system response and the potentially fatal transplant-associated graft-versus-host disease. In donors, two genes were found to significantly increase the risk of cancer-related death in recipients. The investigators also found that mismatch between donors and recipients at several genes, including LINC02774, EPGN, MTHF2DL, and regions in chromosome 4, was associated with an increased risk of all causes of death in the first year after BMT.
The database created during this study will be available publicly, providing an important resource to the global transplant community that can be used for other analyses or further work. Drs. Hahn and Qianqian Zhu, PhD, Associate Professor of Oncology, Department of Biostatistics and Bioinformatics, recently received more than $3 million in grant funding (National Institutes of Health grant R01 CA262899) to extend their analysis and confirm these results in more diverse, multiethnic patient samples that better represent the U.S. transplant population.
The study was supported by the National Institutes of Health (grants R01HL102278 and R03CA188733).
Source: Roswell Park