On the surface, Parkinson's disease -- a neurodegenerative disorder -- and melanoma -- a type of skin cancer -- do not appear to have much in common.
However, for nearly 50 years, doctors have recognised that Parkinson's disease patients are more likely to develop melanoma than the general population.
Now, scientists report a molecular link between the two diseases in the form of protein aggregates known as amyloids.
The researchers will present their results today at the spring meeting of the American Chemical Society (ACS).
ACS Spring 2021 is being held online April 5-30. Live sessions will be hosted April 5-16, and on-demand and networking content will continue through April 30. The meeting features nearly 9,000 presentations on a wide range of science topics.
"Several studies have shown that melanoma occurs two to six times more frequently in the Parkinson's population than the healthy population," says Dexter Dean, Ph.D., a postdoctoral fellow at the National Heart, Lung, and Blood Institute (NHLBI), who is presenting the work at the meeting.
"What's more, the protein involved in Parkinson's disease, α-synuclein, is elevated in melanoma cells."
In Parkinson's disease, α-synuclein forms amyloid deposits that are thought to kill dopamine-producing neurons in the brain, causing symptoms such as tremor, slow movements and dementia.
While intense research has focused on the effects of α-synuclein in the brain, much less is known about its presence or activities in other tissues.
However, scientists have evidence that the amyloid-forming protein is expressed more in melanoma cells than in healthy skin.
Furthermore, higher levels of α-synuclein in melanocytes (the skin cells that give rise to melanoma) correlate with reduced pigment, or melanin, production.
Melanin protects skin from damage by the sun's ultraviolet rays.
Jennifer Lee, Ph.D., Dean's postdoctoral advisor at NHLBI, part of the National Institutes of Health, had previously studied another amyloid-forming protein called premelanosomal protein (Pmel).
"Most people know that amyloids are involved in diseases, such as Parkinson's and Alzheimer's, but it's less well-known that some amyloids, like Pmel, actually serve a useful function," Lee says.
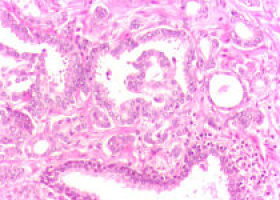
In healthy melanocytes, Pmel forms amyloid fibrils that act as scaffolds to store melanin in melanosomes (the organelle where the pigment is produced, stored and transported).
"Because both α-synuclein and Pmel are expressed in melanoma cells, we wondered if these two amyloid proteins could interact, and whether this interaction could be relevant to the correlation between Parkinson's disease and melanoma," Lee says.
To investigate whether α-synuclein and Pmel could interact, the researchers used microscopy and western blotting to show that the two proteins both resided in the melanosomes of human melanoma cells.
When Dean added preformed α-synuclein amyloid to a test tube containing the amyloid-forming region of Pmel (known as the repeat, or RPT, domain), the α-synuclein fibrils stimulated Pmel to aggregate and form a twisted fibril structure that the protein does not normally adopt on its own.
Because α-synuclein in melanoma cells may also be found in its soluble, or non-amyloid, form, the researchers performed other in vitro experiments in which they added soluble α-synuclein to the Pmel RPT domain.
In this case, α-synuclein inhibited Pmel's ability to self-aggregate and form amyloid in a concentration-dependent manner.
They traced this activity to the first 60 amino acids of α-synuclein.
"We now have preliminary data that suggest an amyloid from one protein can 'seed' or template amyloid from another, and in the soluble form, α-synuclein prevents Pmel aggregation." Lee says.
"Therefore, we think that both forms of α-synuclein could diminish melanin biosynthesis -- the amyloid form by causing Pmel to form an unusual twisted structure, and the soluble form by stopping Pmel from aggregating like it should."
Loss of skin pigmentation could contribute to the increased melanoma risk in Parkinson's disease patients, the researchers say.
"I think we're just at the tip of the iceberg of appreciating what α-synuclein might be doing in melanoma," Dean says. "In future experiments, I'm really interested in understanding more about what α-synuclein is doing to promote melanoma proliferation, in addition to this interaction with Pmel."
Source: American Chemical Society