Diverse diseases like breast cancer can present challenges for clinicians, specifically on a cellular level.
While one patient's tumour may differ from another's, the cells within the tumour of a single patient can also vary greatly.
This can be problematic, considering that an examination of a tumour usually relies on a biopsy, which only captures a small sample of the cells.
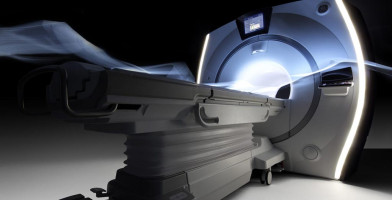
According to a new study from researchers at Penn Medicine, Magnetic Resonance Imaging (MRI) and an emerging field of medicine called radiomics -- which uses algorithms to extract a large amount of features from medical images -- could help to characterise the heterogeneity of cancer cells within a tumour and allow for a better understanding of the causes and progression of a person's individual disease.
The findings were published in Clinical Cancer Research.
"If we're only taking out a little piece of a tissue from one part of a tumour, that does not give the full picture of a person's disease and of his or her response to specific therapies," said principal investigator Despina Kontos, PhD, an associate professor of Radiology in the Perelman School of Medicine at the University of Pennsylvania.
"We know that in a lot of instances, patients are over-treated, getting therapy that may not be beneficial. Or, conversely, patients who need more aggressive therapy may not end up receiving it. The method we currently have for choosing the appropriate treatment for patients with breast cancer is not perfect, so the more steps we can take toward more personalised treatment approaches, the better."
Kontos and her colleagues wanted to determine whether they could use imaging and radiomics for more personalised tumour characterisation.
Using MRI, the researchers extracted 60 radiomic features, or biomarkers, from 95 women with primary invasive breast cancer.
After following up with the patients 10 years later, the group found that a scan that showed high tumour heterogeneity at the time of diagnosis -- meaning a high diversity of cells -- could successfully predict a cancer recurrence.
"Our study shows that imaging has the potential to capture the whole tumour's behaviour without doing a procedure that is invasive or limited by sampling error," said the study's lead author Rhea Chitalia, a PhD candidate in the School of Engineering and Applied Science at the University of Pennsylvania.
"Women who had more heterogeneous tumours tended to have a greater risk of tumour recurrence."
The researchers retrospectively analysed patient scans from a 2002-2006 clinical trial conducted at Penn Medicine.
For each woman, the group generated a "signal enhancement ratio" (SER) map and from it, extracted various imaging features in order to understand the relationship between those features and conventional biomarkers (such as gene mutations or hormone receptor status) and patient outcomes.
They found that their algorithm was able to successfully predict recurrence-free survival after 10 years.
To validate their findings, the group compared their results to an independent sample of 163 patients with breast cancer from the publicly available Cancer Imaging Archive.
While imaging may not completely replace the need for tumour biopsies, radiologic methods could augment what is currently the "gold standard" of care, Kontos said, by giving a more detailed profile of a patient's disease and guiding personalised treatment.
Next steps for the research team will include expanding the analysis to a larger patient cohort and also further exploring which specific markers are more predictive of particular outcomes.
"We've just touched the tip of the iceberg," Kontos said.
"Our results and the validation study give us confidence that there are many opportunities for these markers to be used in a prognostic and potentially a predictive setting."
Source: Perelman School of Medicine
The World Cancer Declaration recognises that to make major reductions in premature deaths, innovative education and training opportunities for healthcare workers in all disciplines of cancer control need to improve significantly.
ecancer plays a critical part in improving access to education for medical professionals.
Every day we help doctors, nurses, patients and their advocates to further their knowledge and improve the quality of care. Please make a donation to support our ongoing work.
Thank you for your support.