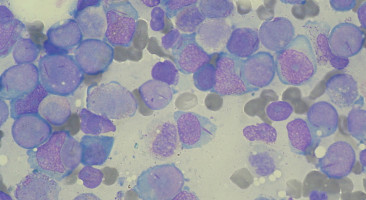
A research team led by Massachusetts General Hospital (MGH) investigators has assembled a detailed atlas of bone marrow cells from patients with acute myeloid leukaemia (AML), an aggressive blood cancer that usually leads to death within five years of diagnosis.
In their study, published in Cell, the team uses advanced technologies to detail both genetic mutations and gene expression in thousands of individual bone marrow cells from AML patients and healthy donors.
Their results reveal specific tumour cell types that resemble normal stages of white blood cell development and also show a role for more differentiated tumour cells in suppressing an anti-tumour immune response.
"Acute myeloid leukaemia is characterised by the accumulation of abnormal white blood cells in the bone marrow and blood of patients, and it has been known for decades that the disease comprises a variety of cell types that resemble normal developmental stages of blood cells," says Peter van Galen, PhD, MGH Department of Pathology and Center for Cancer Research, co-lead author of the Cell paper.
Co-lead author Volker Hovestadt, PhD, also of MGH Pathology and the Center for Cancer Research, adds, "We used new technologies and machine learning to characterise almost 40,000 single cells from the bone marrow of AML patients and healthy volunteers. This approach is providing comprehensive insight into the different types of cancer cells and how they contribute to disease progression."
The researchers used single-cell RNA sequencing to examine gene expression comprehensively in bone marrow cells from 16 AML patients and 5 healthy controls and incorporated a new strategy to determine which cells harboured characteristic AML mutations.
The team then implemented a machine-learning algorithm to distinguish the malignant AML cells from normal cells in the tumour ecosystem.
They found that AML cells could be classified according to their resemblance to six stages of blood cell development.
Moreover, the specific mutations in tumour cells were found to control the developmental stages reflected and also appeared to induce aberrant patterns of gene activity and cell differentiation.
AML cells resembling the earliest stages of development - often called leukaemia stem cells - are known to contribute to disease progression and relapse; and as expected, AML cells expressing genes associated with primitive developmental stages were prominent in patients with poor clinical outcomes.
But the investigators also found evidence that more differentiated AML cells, not previously thought to have a role in tumour progression, can inhibit the function of T cells in the microenvironment, suppressing potential immune responses against the tumour.
"It is now clearer that genetic mutations can drive different cancer cell types that need to be specifically targeted with precision therapies, so our findings can guide personalised therapies to eradicate AML cells," says van Galen.
"Immune therapies that harness T cells have been less successful in AML, and our findings suggest that their efficacy could be improved by overcoming the inhibitory signals from differentiated tumour cells. Finally, better understanding of the abnormal regulation of developmental genes in leukaemia stem cells may provide fundamental insights into the origins of this disease."
Senior author Bradley Bernstein, MD, PhD, MGH Pathology and Center for Cancer Research adds, "This study would not have been possible without an incredible interdisciplinary team of cancer biologists, clinicians, technologists and computational scientists from MGH, the Ludwig Center at Harvard, the Broad Institute, and the Dana-Farber Cancer Institute. This collaboration to advance our understanding of cancer cell biology has the potential to significantly improve therapies for patients with what has been a very difficult to treat disease."
Source: Massachusetts General Hospital