A new immunotherapy screening prototype developed by University of California, Irvine researchers can quickly create individualised cancer treatments that will allow physicians to effectively target tumours without the side effects of standard cancer drugs.
UCI's Weian Zhao and Nobel laureate David Baltimore with Caltech led the research team that developed a tracking and screening system that identifies T cell receptors with 100-percent specificity for individual tumours within just a few days.
Research findings appear in Lab on a Chip.
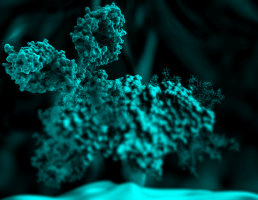
In the human immune system, T cells have molecules on their surfaces that bind to antigens on the surface of foreign or cancer cells.
To treat a tumour with T cell therapy, researchers must identify exactly which receptor molecules work against a specific tumour's antigens.
UCI researchers have sped up that identification process.
"This technology is particularly exciting because it dismantles major challenges in cancer treatments," said Zhao, an associate professor of pharmaceutical sciences who is affiliated with the Chao Family Comprehensive Center and the Sue & Bill Gross Stem Cell Research Center.
"This use of droplet microfluidics screening significantly reduces the cost of making new cancer immunotherapies that are associated with less systemic side effects than standard chemotherapy drugs, and vastly speeds up the timeframe for treatment."
Zhao added that traditional cancer treatments have offered a one-size-fits-all disease response, such as chemotherapy drugs which can involve systemic and serious side effects.
T cell receptor (TCR)-engineered T cell therapy, a newer technology, harnesses the patient's own immune system to attack tumours.
On the surface of cancer cells are antigens, protruding molecules that are recognised by the body's immune system T cells.
This new therapy places engineered molecules on the patient's T cells which will bind to their cancer cell antigens, allowing the T cell to destroy the cancer cell.
TCR therapy can be individualised, so each patient can have T cells designed specifically for their tumour cells.
This antigen-TCR recognition system is very specific - there can be hundreds of millions of different types of TCR molecules.
A big challenge for TCR-T cell therapy development remains in identifying particular TCR molecules out of a pool of millions of possibilities.
Finding a match can take up to a year (time many cancer patients don't have) and can cost half a million dollars or more per treatment.
By using miniscule oil-water droplets, Zhao's team designed a device that allows for individual T cells to join with cancer cells in microscopic fluid containers.
The TCRs that bind with the cancer cells' antigens can be sorted and identified within days, considerably faster than the months or year that previous technologies required.
The technology also significantly reduces the cost of making individualised TCRs and accelerates the pipeline of TCR-T cell therapy to clinic.
Through a partnership with Amberstone Biosciences, a UCI start-up, this entire platform and screening process will be available to pharmaceutical companies for drug development within just a few months.
Not only can this technology help revolutionise TCR-T cell therapies for cancer, but it will also be a powerful tool for discovering other immunological agents, including antibodies and CAR-T cells, and for elucidating new immunology and cancer biology at a depth not possible before.
Source: UCI