Two recent studies in the journal Leukaemia present a new approach for bone marrow donation and transplant that preclinical laboratory tests suggest could make the life-saving procedure safer and more effective for patients.
Researchers at the Cincinnati Children's Cancer and Blood Diseases Institute say their studies demonstrate that use of an experimental drug called CASIN in laboratory mice results in higher efficiency when harvesting blood stem cells from donors and less toxicity in transplant recipients.
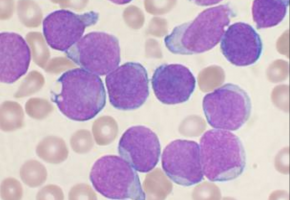
Designed to repair the body's blood-making machinery inside the bone marrow, a stem cell transplant can be life-saving for people with cancers like leukaemia or those battling immune deficiency diseases.
But prepping patients for transplant involves using toxic chemotherapy to kill off a person's existing and malfunctioning blood-making system.
This allows it to be replaced with healthy blood stem cells called haematopoietic stem cells (HSCs).
In addition to toxicity for patients, the procedure doesn't always work.
According to Yi Zheng, PhD, senior investigator on both studies and director of Experimental Haematology and Cancer Biology, harvesting effective donor HSCs can be a challenge and, once transplanted, the cells often do not engraft in sufficient numbers to make the patient healthy,
In one Leukaemia study, Zheng's team rationally designed the drug CASIN.
The drug mimics the action of an important gene called CDC42 that helps regulate blood stem cells.
Tests in mouse models show that CASIN can effectively mobilise blood-making stem cells and promote their exit from the bone marrow.
The study indicates that blood stem cells harvested from CASIN-treated donor mice have better long-term reconstitution potential following transplant than cells harvested with regimens currently used in clinic.
In the second study, researchers used CASIN to precondition mouse transplant recipients to make the body's bone marrow compartments more receptive to new and healthy blood stem cells.
The drug does this by prompting existing blood stem cells to vacate the bone marrow and migrate to peripheral blood, which is located in circulating blood not sequestered to the bone marrow.
This lessens the amount of chemotherapy needed to precondition the bone marrow in transplant recipients.
It could allow effective transplant preconditioning when a recipient is unable to tolerate a chemotherapy-based procedure.
"Our data demonstrate that the new regimen of CASIN application has the potential to improve both sides of the transplant practice. It mobilises higher quality donor HSCs during stem cell harvest and it would condition transplant patients beforehand to increase engraftment efficiency," Zheng said. "This would be a major step forward, especially for the most vulnerable patients who cannot withstand the toxicity of chemotherapy conditioning regimens or are non-responsive to current blood-stem-cell mobilisation regimens."
CASIN works by modulating the function of the CDC42 gene's target protein, Cdc42 (cell division control protein 42).
In blood stems cells Cdc42 levels are tightly controlled and altering its activity can cause a transient change in function and movement of HSCs.
Zheng and his colleagues explain that careful control of Cdc42 activity during stem cell donation and bone marrow transplant produces the benefits of 1) high-quality stem cells harvested from donors and 2) improved preconditioning for transplant recipients.
Although Zheng said the laboratory findings establish a proof of principle for the new regimen, the researchers caution the procedure using CASIN remains in pre-clinical testing.
The current study was conducted in donated human cells, mouse cells and mouse models of bone marrow transplant.
Results in such studies don't always translate to human patients.
Source: Cincinnati Children's Hospital Medical Center