Previous research has revealed that patients with acute myeloid leukaemia who also have a particular mutation in a gene called NPM1 have a higher rate of remission with chemotherapy.
About one-third of leukaemia patients possess this favourable mutation, but until now, how it helps improve outcomes has remained unknown.
Scientists from the University of Illinois at Chicago report on how this mutation helps improve sensitivity to chemotherapy in patients in the journal JCI Insight.
The protein coded for by the NPM1 gene affects the location and activity of another protein called FOXM1.
FOXM1 activates other cancer-promoting genes and has been found to be elevated in cancer cells.
The presence of FOXM1, especially at high levels, is a strong predictor of worse treatment outcomes and decreased survival in patients with cancer.
When the NPM1 gene is mutated, FOXM1 can't activate additional oncogenes, so patients with this mutation tend to respond better to chemotherapy.
A drug that targets and incapacitates FOXM1 in patients without the beneficial NPM1 mutation may help improve the efficacy of chemotherapy.
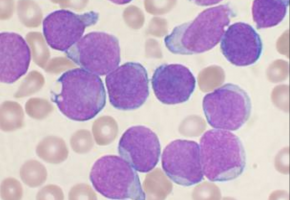
Acute myeloid leukaemia (AML) is a cancer of the bone marrow.
In AML, stem cells that would normally differentiate into blood cells instead multiply unchecked and fail to develop into mature blood cells.
Patients with AML have a high risk of death from uncontrolled infection, fatigue easily and get organ damage because they lack adequate numbers of oxygen-carrying red blood cells.
They are also at high risk for dangerous bleeding because of low numbers of cells that help with blood clotting.
It has been known that patients with a mutation in the NPM1 gene have a better response to standard chemotherapy, with up to 80 percent of patients being cured compared to just 40 percent for patients without the mutation.
In previous studies, researchers at UIC led by Andrei Gartel, associate professor of molecular genetics, discovered that one of the roles of the NPM protein is to stabilize FOXM1 and keep it in the nucleus where it can activate other cancer-promoting genes.
Gartel and his colleagues determined that when the NPM1 gene is mutated, FOXM1 migrates out of the nucleus and into the cell's cytoplasm, where it can't interact with DNA.
This may explain why patients with this NPM1 mutation have a much better response to chemotherapy and are less likely to relapse.
In their current study, Gartel and his colleagues further explored the relationship between NPM1 and FOXM1 in patients with AML.
The researchers analyzed bone marrow cells taken via biopsies from 77 patients with AML and found that the presence of FOXM1 in the cells' nuclei was a strong predictor of poor treatment outcome for individual patients.
"When we then looked in the patients' medical records, we saw that those with FOXM1 present in the nucleus of their cancer cells had worse treatment outcomes, higher rates of chemotherapy resistance and lower survival rates compared to patients without FOXM1 present in the nucleus," said Dr. Irum Khan, assistant professor of clinical medicine in the UIC College of Medicine and first author on the paper.
In mice engineered to overproduce FOXM1 that were caused to develop leukaemia, following treatment with cytarabine, a drug commonly used to treat AML, the mice had more residual disease compared to control mice with AML and normal levels of FOXM1.
"Our finding suggests that overexpression of FOXM1 directly induces chemoresistance, which matches what we saw in our analysis of patients' FOXM1 levels and their treatment outcomes," said Khan.
Next, the researchers demonstrated that they could produce a therapeutic response in patient AML cells grown in the lab using a novel oral drug called ixazomib, which is approved to treat another form of cancer called multiple myeloma.
In the current paper, Gartel and his colleagues show that ixazomib works in part by suppressing FOXM1.
When the patient cancer cells were treated with ixazomib plus standard chemotherapy drugs used to treat AML (cytarabine and anthracyclines) the cells showed a higher death rate compared with standard chemotherapy alone. "Ixazomib produced a synergized chemotherapeutic response when added to standard chemotherapy," Gartel said. "We believe this is caused by ixazomib inhibiting the activity of FOXM1."
"There is a real unmet need for new ways to get around the resistance to chemotherapy that patients who don't have this beneficial mutation often face," said Khan. "Drugs that suppress FOXM1 in combination with the standard treatment, such as ixazomib, should result in better outcomes, but clinical trials will ultimately be needed to prove this theory."
Source: University of Illinois at Chicago
The World Cancer Declaration recognises that to make major reductions in premature deaths, innovative education and training opportunities for healthcare workers in all disciplines of cancer control need to improve significantly.
ecancer plays a critical part in improving access to education for medical professionals.
Every day we help doctors, nurses, patients and their advocates to further their knowledge and improve the quality of care. Please make a donation to support our ongoing work.
Thank you for your support.