Scientists have discovered that it is possible to identify people at high risk of developing acute myeloid leukaemia (AML) years before diagnosis.
The researchers from Wellcome Sanger Institute, European Bioinformatics Institute (EMBL-EBI) and their international collaborators found that patients with AML had genetic changes in their blood years before they suddenly developed the disease.
The study, published in the journal Nature, found that blood tests looking for changes in the DNA code can reveal the roots of AML in healthy people.
Further research could allow earlier detection and monitoring of people at risk of AML in the future, and open the prospect of developing ways to reduce the likelihood of developing this cancer.
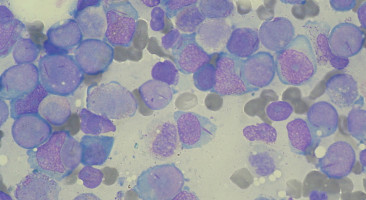
Acute myeloid leukaemia is an aggressive blood cancer that affects people of all ages.
The cancer cells multiply quickly in the bone marrow and stop the production of normal blood cells, leading to fatal infections and bleeding.
Mainstream treatments for AML treatments have changed very little for several decades and whilst some patients are cured, the majority are not.
To uncover the earliest steps in the development of AML, the researchers collaborated with the European Prospective Investigation into Cancer and Nutrition (EPIC) study*.
Enrolment into EPIC started in 1992 and a large number of people have been enrolled and followed up for cancer development, with lifestyle data and blood samples collected.
Some of these people later developed AML and, using their stored blood samples, the researchers were able to look back in time to see which genetic changes were already present years before the disease appeared.
The scientists, including researchers from the Princess Margaret Cancer Centre in Canada and the Weizmann Institute in Israel, sequenced the stored blood DNA from 124 AML patients and compared it to that from 676 people who remained free from AML or a related cancer.
Remarkably, they discovered that many of the people that went on to develop AML had particular genetic changes that set them apart from those who did not. These changes could be used collectively to develop a predictive test for AML risk.
Dr Grace Collord, joint first author on the paper from the Wellcome Sanger Institute and University of Cambridge, said: "Acute myeloid leukaemia often appears very suddenly in patients, so we were surprised to discover that its origins are generally detectable more than five years before the disease develops. This provides proof-of-principle that it may be possible to develop tests to identify people at a high risk of developing AML."
The study focussed on selected genes known to be associated with AML, and found frequent mutations in some of these genes in many individuals, including some people that did not develop AML.
However, the researchers discovered that people who were en-route to developing AML had a higher number of mutations and that the mutations were often present in a larger fraction of their blood cells.
Furthermore, specific blood test results were subtly different in those who later developed AML.
Dr Moritz Gerstung, one of the senior authors on the paper from the EBI, said: "We needed a large number of samples to get accurate results, and this study was only possible through a collaboration with the European Prospective Investigation in Cancer and Nutrition (EPIC). The generosity of the participants in sharing their data and blood samples allowed us to discover a pattern of genetic changes that is established long before AML appears, and which confers greater risk when more cells are affected by genetic change. This genetic lag may also be found in other blood cancers, and this would open new avenues for further research that could help many people in the future."
Approximately 5 in 100,000 people in the general population develop AML each year.
This means that any predictive tests need to be highly accurate in order to minimise the risk of false positive results.
Despite the powerful methods used in the study, further research will be needed to enhance the accuracy of predictive tests to make them robust enough to use clinically.
The aim is to identify individuals at risk of AML and monitor them closely, whilst developing approaches for preventing leukaemia development.
Dr George Vassiliou, one of the joint leaders of the project from the Wellcome Sanger Institute and the Wellcome-MRC Cambridge Stem Cell Institute, and Consultant Haematologist at Cambridge University Hospitals NHS Trust, said: "Our study provides for the first time evidence that we can identify people at risk of developing AML many years before they actually develop this life-threatening disease. We hope to build on these findings to develop robust screening tests for identifying those at risk and drive research into how to prevent or stall progression towards AML. Our aspiration is that one day AML prevention would provide a compelling alternative to treatment."
Source: Wellcome Trust Sanger Institute
We are an independent charity and are not backed by a large company or society. We raise every penny ourselves to improve the standards of cancer care through education. You can help us continue our work to address inequalities in cancer care by making a donation.
Any donation, however small, contributes directly towards the costs of creating and sharing free oncology education.
Together we can get better outcomes for patients by tackling global inequalities in access to the results of cancer research.
Thank you for your support.