Using a mathematical modelling approach, scientists have found that certain parameters of tumour growth in mice can predict the effectiveness of drugs that block formation of tumour-nourishing blood vessels.
The findings are published in PLOS Computational Biology.
Even within the same cancer type, different tumours can respond differently to cancer drugs, and some tumours do not respond at all.
Therefore, it is useful to identify tumour features that can serve as "predictive biomarkers" to forecast how a person's tumour might respond to a particular treatment.
However, before drugs are tested in humans in a clinical setting, they are usually explored in mice.
In efforts to enhance pre-clinical drug testing, Thomas Gaddy of the University of Southern California, Los Angeles, and colleagues in the research group of Professor Stacey Finley investigated a potential predictive biomarker for a type of cancer drug known as anti-angiogenic therapy.
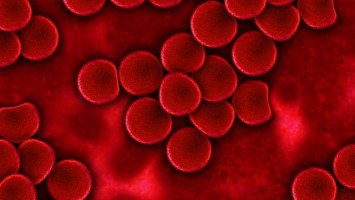
This treatment inhibits the formation of new blood vessels that can help a tumour grow.
The researchers had previously built a mathematical model that simulates the activity of a blood-vessel-growth-promoting protein called VEGF in a mouse tumour.
For the new study, they added a component to the model that simulates the tumour's response to drugs that target VEGF and inhibit its activity.
They trained and validated the model using real-world data on tumour growth in mice.
Using their new model, the researchers found that certain parameters about the way a tumour grows could successfully and accurately predict its response to anti-angiogenic treatment that targets VEGF activity.
Using those characteristics, they were able to predict how effective the treatment would be (i.e., whether tumour growth would slow), even before the start of treatment.
If these results are confirmed in live mouse studies, they could eventually lead to new strategies to predict tumour response to anti-angiogenic therapy in people.
Meanwhile, the research team is using their model to simulate such a study.
"In our virtual mouse study, we will simulate tumour growth with and without treatment and determine if the growth parameters can indeed be used to distinguish between mice whose tumours will respond to therapy or not," Finley says. "We are also scouring published literature to find more experimental data to further validate our model predictions."
Source: PLOS
We are an independent charity and are not backed by a large company or society. We raise every penny ourselves to improve the standards of cancer care through education. You can help us continue our work to address inequalities in cancer care by making a donation.
Any donation, however small, contributes directly towards the costs of creating and sharing free oncology education.
Together we can get better outcomes for patients by tackling global inequalities in access to the results of cancer research.
Thank you for your support.