Patients with advanced Hodgkin lymphoma (HL) who were treated with a multi-drug regimen that included the targeted agent brentuximab vedotin (BV) had a 23-percent reduction in the risk of disease progression, death, or the need for additional therapy, compared with patients who received the standard four-drug first-line regimen for treating advanced HL, researchers reported.
This data was presented in a press conference at the 2017 ASH annual meeting.
For more information watch our interview with Dr Joseph Connors.
In this multinational, Phase III clinical trial, the addition of BV to standard treatment improved patients’ chances of being cured with the first round of treatment, avoiding the need for additional, more intensive therapy.
The study results represent the first successful effort in more than 30 years to improve outcomes of first-line treatment in patients with advanced HL without escalating the toxicity of the chemotherapy to unacceptable levels, said lead study author Joseph M. Connors, MD, clinical director of the British Columbia Cancer Agency Centre for Lymphoid Cancer in Vancouver, Canada.
Standard treatment for HL, consisting of the drugs Adriamycin (doxorubicin), bleomycin, vinblastine, and dacarbazine (ABVD), has not changed since the 1970s, said Dr. Connors, adding that previous trials have failed to improve the outcomes achieved with ABVD without causing severe side effects.
“We expect ABVD to cure about three-quarters of patients — which means, of course, that one quarter will not be cured,” he explained.
“In this study we’ve been able to significantly reduce that rate of treatment failure. If this new regimen is widely adopted, it will change first-line treatment of advanced HL.”
BV works by first attaching to the surface of HL cells, then entering the cells to deliver a toxic substance, he said.
This is the first time a drug designed to take advantage of a specific biologic characteristic of HL cells has been used in first-line treatment of the disease, he said.
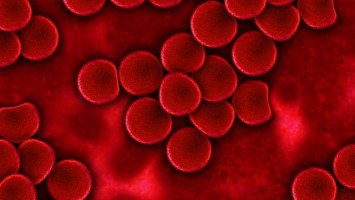
HL originates in white blood cells and commonly occurs in young people.
An estimated 8,200 cases will be diagnosed in the United States in 2017.
The average age at diagnosis is 39.
In about two-thirds of patients, the disease has spread widely throughout the body at diagnosis.
If first-line therapy fails, patients must undergo a second round of more intensive treatment.
In the study, 1,334 patients with previously untreated advanced HL were randomly assigned to receive either ABVD or BV plus doxorubicin, vinblastine, and dacarbazine (AVD), with up to 50 months’ follow-up.
Treatment was deemed to have failed if patients’ lymphoma did not completely disappear or if its persistence prompted additional non-study treatment.
Although the experimental combination of BV and AVD caused more nerve damage, episodes of fever, and neutropenia (low levels of infection-fighting white blood cells) than ABVD, the nerve damage largely reversed during follow-up and the rate of serious infections could be kept to low levels with the use of medication to encourage infection-fighting white blood cells to recover more quickly, according to Dr. Connors.
The experimental combination of BV and AVD meant patients didn’t receive bleomycin, which has been linked to lung damage and sometimes death.
“The experimental combination with BV more frequently got rid of all of the disease, and this was achieved with acceptable levels of adverse effects,” said Dr. Connors.
“Treatment with BV was modestly more toxic, but when we added simple measures to improve patients’ blood counts, they were able to take it safely.”
Source: ASH 2017
The World Cancer Declaration recognises that to make major reductions in premature deaths, innovative education and training opportunities for healthcare workers in all disciplines of cancer control need to improve significantly.
ecancer plays a critical part in improving access to education for medical professionals.
Every day we help doctors, nurses, patients and their advocates to further their knowledge and improve the quality of care. Please make a donation to support our ongoing work.
Thank you for your support.