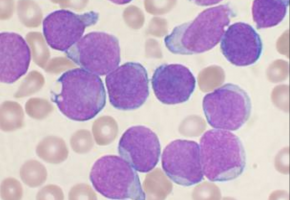
Notch is one of the most frequently mutated genes in chronic lymphocytic leukaemia (CLL), the most common leukaemia in adults in the United States.
It is also often mutated in other common B cell tumours, such as mantle cell lymphoma.
However, the role of Notch in these cancers has been uncertain.
Now, a collaborative effort between investigators at the Perelman School of Medicine at the University of Pennsylvania and the Harvard Medical School provides new insights into how Notch drives the growth of B-cell cancers.
The teams report their findings in Cell Reports.
The researchers found that in B cell tumours, mutated overactive versions of the Notch protein directly drive the expression of the Myc gene and many other genes that participate in B cell signalling pathways.
Myc is a critical gene in governing cell proliferation and survival, activities that it carries out by regulating the expression of other genes involved in cell metabolism.
B cell signalling pathways are the current targets of several therapies used to treat B cell malignancies such as CLL.
"An important translational implication of this research is that we hope that by combining Notch inhibitors with drugs that target B-cell signalling we can better treat these B-cell cancers," said senior author Warren Pear, MD, PhD, a professor of Pathology and Laboratory Medicine at Penn Medicine. "Although this is true of many transcription factors, it has been difficult to develop therapeutics that directly target the Myc protein, an alternative approach may be to target the proteins that regulate Myc expression."
Notably, multiple Notch inhibitors are in various stages of clinical development as potential cancer therapies.
The mechanism used by Notch to regulate Myc in B cells is distinct from the mechanism used in other cell types, such as T cells, where Notch also regulates Myc.
The team found that Notch uses different regulatory switches in the genome, called enhancers, in different cell types.
This raises the issue of why evolution would select for this complexity.
One reason may be that Myc needs to be under very tight control in each cell.
For example, in the mouse model of Notch-induced T-cell leukaemia, the Penn group previously found that the difference between inducing a T cell tumour or not is a doubling of Myc transcription by Notch.
As Notch appears to use cell type-specific machinery to regulate Myc, it may be possible to target the Notch-Myc signalling path in a way that does not disrupt this path in other cell types.
Another surprising finding was the direct link between Notch and genes involved in other B cell signalling pathways.
For example, Notch activates genes involved in B cell receptor signalling, which is an established drug target in these B cell cancers.
The challenge now will be to understand what this might mean for treatment of patients with Notch-activated B-cell leukaemias and lymphomas.
The team plans to test the synergy between Notch and B-cell signalling inhibitors.
If they find a relationship, the next step would be to stimulate interest in a clinical trial.
Source: Perelman School of Medicine - University of Pennsylvania
The World Cancer Declaration recognises that to make major reductions in premature deaths, innovative education and training opportunities for healthcare workers in all disciplines of cancer control need to improve significantly.
ecancer plays a critical part in improving access to education for medical professionals.
Every day we help doctors, nurses, patients and their advocates to further their knowledge and improve the quality of care. Please make a donation to support our ongoing work.
Thank you for your support.