Genomic testing of tumour samples can enable personalised treatment selection, where targeted treatments are matched to genetic changes in the tumour.
Although a growing number of patients with advanced cancers receive some genomic testing, comprehensive genomic testing is not yet routine care.
A study in France of 1,944 patients with advanced cancer suggests that widespread, routine genomic testing is feasible, although it offers clinical benefit to only of subset of patients at this time.
According to the authors, this is the largest study of its kind.
The study was presented at the 2017 American Society of Clinical Oncology (ASCO) Annual Meeting.
The researchers found least one “actionable” alteration in 52% of the tumour samples tested (“actionable” alterations are genetic changes that theoretically can be matched to targeted therapies).
A molecular tumour board recommended targeted treatments to 676 patients, and 143 of them received the recommended treatment.
The five-year survival rate was higher among patients who received the recommended treatment than among those who did not (34.8% vs. 28.1%).
“This study confirms that comprehensive genomic profiling can be performed in routine practice to select patients for targeted cancer therapies,” said lead study author Olivier Tredan, MD, PhD, chair of the Department of Medical Oncology at the Centre Léon Bérard in Lyon, France. “The technology is widely available and requires only a small amount of DNA. Theoretically, we could do this testing for every patient in France.”
About the Study
ProfiLER is an ongoing clinical trial that uses genomic profiling of tumours to guide treatment decisions for patients with advanced cancer.
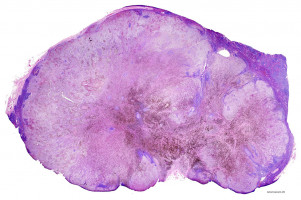
DNA from tumour samples is analysed by next-generation sequencing of 69 cancer-related genes and whole-genome-comparative genomic hybridization.
Both technologies are widely available in France and elsewhere in the world, according to the authors.
A multidisciplinary board of experts (the molecular tumour board) meets weekly to review genomic testing results and, if actionable mutations are found, provides recommendations for molecularly targeted therapies.
“We recommended molecularly targeted therapies to patients who had mutations in pathways that could be targeted with either commercially available drugs or those tested in early clinical trials,” said Dr. Tredan.
Key Findings
To date, 2,676 patients have enrolled in the study, and 1,944 tumours were analysed, including colorectal, gynecologic, breast, brain, and head and neck cancer, as well as sarcoma.
Actionable mutations were found in 1,004 (52%) of tumour samples; 609 patients had only one actionable mutation, and 394 had two or more (up to six). The most common actionable pathway was the PI3K/mTOR pathway.
The molecular tumour board recommended molecularly targeted treatments to 676 patients (35% of 1,944 tested) based on availability of drugs hitting either the target protein or the pathway activated by the target.
Of those, 143 received the recommended treatment, most through enrollment in a clinical trial.
The other 533 patients were not able to receive the recommended treatment because of poor health/rapid progression of the cancer, not meeting eligibility criteria for a clinical trial, or difficulty obtaining off-label commercial medicines.
Researchers compared overall survival rates for the 143 patients who received targeted therapies based on genomic testing and 502 patients who did not.
At three years, 53.7% of patients who received the recommended targeted therapy were alive, compared to 46.1% of patients who did not.
The five-year survival rate was also higher for patients who received targeted therapy (34.8% vs. 28.1%).
Next Steps
The researchers are planning a new, randomised clinical trial, ProfiLER 02, which will compare the 70-gene test used in the current study to a commercial, 315-gene test.
That trial should reveal whether screening a larger number of genes leads to more recommendations for targeted therapy.
Watch the press conference here.
Source: ASCO 2017
We are an independent charity and are not backed by a large company or society. We raise every penny ourselves to improve the standards of cancer care through education. You can help us continue our work to address inequalities in cancer care by making a donation.
Any donation, however small, contributes directly towards the costs of creating and sharing free oncology education.
Together we can get better outcomes for patients by tackling global inequalities in access to the results of cancer research.
Thank you for your support.