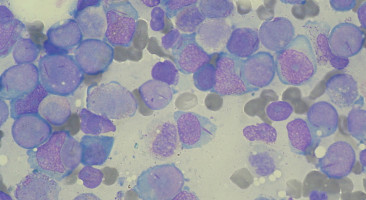
Columbus, Ohio - An international panel of experts has released updated evidence-based and expert-opinion-based recommendations for the diagnosis and treatment of acute myeloid leukaemia (AML) in adults.
The recommendations were issued by the European LeukaemiaNet (ELN) and published in the journal Blood.
The paper's senior author was Clara D. Bloomfield, MD, Distinguished University Professor, Ohio State University Cancer Scholar and Senior Adviser, and the William Greenville Pace III Endowed Chair in Cancer Research.
"These guidelines are an important update of the current and widely used recommendations for managing AML, for constructing clinical trials and for predicting outcomes of AML patients," says Bloomfield, who co-chaired the panel. "They will be the new standard of care and will replace the 2010 ELN recommendations for managing AML patients and designing clinical trials."
Adult AML affects an estimated 21,400 Americans per year and kills 10,600 of them, according to the American Cancer Society.
The updated recommendations include revised ELN genetic categories, a proposed response category based on minimal residual disease status, and a proposed category for progressive disease for clinical trials.
They also include the newly updated World Health Organisation classification of myeloid neoplasms and acute leukaemia, also published in the journal Blood.
Bloomfield said updating the ELN recommendations was prompted by new insights into the molecular and genomic causes of the disease, by the development of new genetic tests and tests for detecting minimal residual disease and by the development of novel anti-leukaemic agents.
The panel that produced the new guidelines included 22 international members with recognised AML clinical and research expertise. Bloomfield notes three particularly significant changes in the updated ELN recommendations:
We are an independent charity and are not backed by a large company or society. We raise every penny ourselves to improve the standards of cancer care through education. You can help us continue our work to address inequalities in cancer care by making a donation.
Any donation, however small, contributes directly towards the costs of creating and sharing free oncology education.
Together we can get better outcomes for patients by tackling global inequalities in access to the results of cancer research.
Thank you for your support.