Cancer cells love glucose, the simple sugar the body uses for energy, so a high-fat, low-carb diet should starve them, right?
Not so fast.
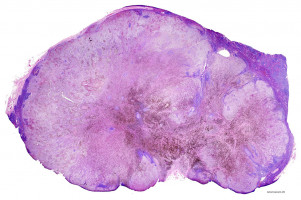
Research in mice suggests that melanomas and other cancers driven by a particular mutation (BRAF V600E) will grow faster in response to a high-fat diet.
In addition, lipid-lowering agents such as statins curb these cancers' growth, even in the context of a more normal diet.
The results are scheduled for publication in Cell Metabolism.
While the findings cover only one mutation and need to be tested clinically, they sketch out the concept of a "precision diet," tailored to an individual patient's cancer.
"While human cancers share some common metabolic properties, they may also have distinct sensitivities depending on their oncogenic mutation profiles," says senior author Jing Chen, PhD, professor of haematology and medical oncology at Winship Cancer Institute of Emory University. "For certain mutations, it could be possible to design dietary regimens that may prevent or delay tumour progression."
Most cancer cells display enhanced glucose uptake, a phenomenon known as the Warburg effect.
A low-carb diet has been tried as a clinical countermeasure in a limited way, mainly in brain cancer.
In contrast, a possible implication of the Winship researchers' results is that people fighting a cancer with a BRAF V600E mutation should avoid low-carb diets.
This mutation is found in more than 60 percent of melanomas and all of the hairy cell type of leukaemia, as well as a subset of colorectal cancers (10 percent) and multiple myelomas (5 percent).
Drugs are available that target the BRAF V600E mutation, but resistance to the drug usually develops.
Chen's lab, working with Sumin Kang, PhD and colleagues at Winship, had previously discovered that the V600E mutation rewires cancer cells' metabolism, stimulating the ketogenesis pathway.
Through ketogenesis, the body breaks down fats for energy when glucose levels in the blood are low.
One of the alternative energy sources produced by ketogenesis is acetoacetate.
Within cancer cells with the V600E mutation, acetoacetate production is stimulated, the Winship researchers had found.
On top of that, acetoacetate binds the mutated B-raf protein and promotes its oncogenic activity, forming a cycle of positive feedback.
The Winship researchers wanted to test whether V600E cancer cells would respond to external acetoacetate.
A ketogenic diet with very low carbohydrates, like an Atkins diet, can cause acetoacetate levels in the body to rise.
Fasting can also trigger the same effect.
When researchers fed mice a diet with more than 90 percent of its calories from fat, grafted tumours derived from V600E melanoma cells grew faster (twice as large over four weeks) than in mice fed a normal diet.
This was not true of tumours derived from melanoma cells with other oncogenic mutations.
Lipid-lowering agents commonly used to treat high cholesterol, such as statins (in this case, fluvastatin), niacin and fenofibrate, could slow the expansion of V600E tumours in mice, even when they were fed a normal diet.
Those drugs reduced acetoacetate levels, and when the researchers injected acetoacetate to compensate, tumour growth sped up again.
"Limiting dietary fat intake and monitoring circulating acetoacetate levels might be beneficial in patients with BRAF V600E melanoma or other related cancers," Chen says. "At this point, we can't be specific about diet suggestions, because we need to know more about what types of dietary fat trigger acetoacetate production."
"Lipid lowering agents may have a role in cancer prevention or supplemental treatment approaches to reduce cancer progression or improve clinical outcomes in the BRAF V600E-positive pre-malignancy and cancer settings," Chen adds.
The researchers showed that a chemical that structurally resembles acetoacetate, dehydroacetic acid, inhibits acetoacetate's effects on V600E tumour growth.
Dehydroacetic acid is used in cosmetics and appears to have low toxicity, but clinical studies would be needed to assess its anticancer properties, especially at the levels that could alter cell metabolism.
Source: Emory Health Sciences