Data has been presented from an ongoing phase 1 clinical trial evaluating SGN-LIV1A for patients with metastatic breast cancer (MBC), with particular focus on triple-negative MBC (TN MBC), at the 39th San Antonio Breast Cancer Symposium (SABCS).
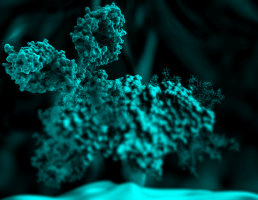
SGN-LIV1A is an investigational antibody-drug conjugate (ADC) which consists of a LIV-1-targeted monoclonal antibody linked to the cell-killing agent monomethyl auristatin E (MMAE) by a protease-cleavable linker.
LIV-1 is a protein expressed by most metastatic breast cancers.
SGN-LIV1A is one of four clinical-stage empowered antibody therapies under development by Seattle Genetics for solid tumours.
SGN-LIV1A consists of a LIV-1-targeted monoclonal antibody linked to a potent microtubule-disrupting agent, monomethyl auristatin E (MMAE) by a protease-cleavable linker, using the same technology as brentuximab vedotin.
It is designed to bind to LIV-1 on cancer cells and release the cell-killing agent into target cells upon internalisation.
SGN-LIV1A may also cause antitumor activity through other mechanisms, including activation of an immune response.
Interim data from the ongoing phase 1 study of SGN-LIV1A in patients with MBC were previously presented at the 2015 SABCS.
The following updated results from this trial describe safety data for all patients and antitumor activity data for patients with TN MBC.
Data were reported from 53 patients with LIV-1-expressing MBC who were treated with SGN-LIV1A monotherapy administered every three weeks. Of these patients, 35 had TN MBC.
The median age of all patients was 56 years.
Patients had received a median of four prior systemic therapies for metastatic disease.
Key findings presented by Dr. Andres Forero-Torres, University of Alabama at Birmingham included that thirty of 47 efficacy-evaluable patients had TN MBC.
Among these patients, 11 (37 percent) achieved a partial response (PR).
The disease control rate (DCR) was 67 percent and the clinical benefit rate (CBR) was 47 percent.
DCR is defined as patients achieving a complete response (CR), PR or stable disease (SD).
CBR is defined as patients achieving CR or PR of any duration plus patients achieving SD lasting at least 24 weeks.
At the time of this interim data analysis, the estimated median progression-free survival for TN MBC patients was 12 weeks with seven patients remaining on treatment.
The maximum tolerated dose was not reached among doses ranging from 0.5 to 2.8 milligrams per kilogram (mg/kg).
Dose escalation is complete and a disease-specific expansion cohort of TN MBC patients is currently enrolling.
For all patients in the study, the most common adverse events of any grade occurring in 20 percent or more of patients included fatigue (57 percent), nausea (53 percent), alopecia (42 percent), decreased appetite (34 percent) and constipation (32 percent).
The incidence of grade 3/4 neutropenia at the 2.5 mg/kg dose was 50 percent.
Two patients (seven percent) experienced febrile neutropenia, and there was one treatment-related death due to sepsis.
Based on these safety data, a separate expansion cohort at 2.0 mg/kg is currently being evaluated.
Peripheral neuropathy events occurred in 38 percent of patients and were generally low grade and manageable.
Enrollment continues for patients with TN MBC in the SGN-LIV1A monotherapy part of the study.
In addition, enrollment is ongoing for patients with HER2 breast cancer to evaluate SGN-LIV1A in combination with trastuzumab.
“Breast cancer is the most common cancer among women, with an estimated 1.67 million new cases per year worldwide. About 15 to 20 percent of breast cancers are triple negative, which means they lack expression of three breast cancer-associated proteins that serve as key therapeutic targets. Triple-negative breast cancers are more aggressive and generally have poor prognoses,” said Jonathan Drachman, M.D., Chief Medical Officer and Executive Vice President, Research and Development at Seattle Genetics. “The data presented at SABCS on SGN-LIV1A demonstrate promising early antitumor activity with a 37 percent partial response rate in patients with triple negative metastatic breast cancer, for which there are no available targeted treatments. We are enrolling additional patients with triple negative metastatic breast cancer in our phase 1 study to optimise the dose and inform the next steps for development of SGN-LIV1A in this population with high unmet need.”
Source: SABCS 2016
The World Cancer Declaration recognises that to make major reductions in premature deaths, innovative education and training opportunities for healthcare workers in all disciplines of cancer control need to improve significantly.
ecancer plays a critical part in improving access to education for medical professionals.
Every day we help doctors, nurses, patients and their advocates to further their knowledge and improve the quality of care. Please make a donation to support our ongoing work.
Thank you for your support.