A major challenge in truly targeted cancer therapy is cancer's suppression of the immune system.
Northwestern University synthetic biologists now have developed a general method for "rewiring" immune cells to flip this action around.
"Right now, one of the most promising frontiers in cancer treatment is immunotherapy -- harnessing the immune system to combat a wide range of cancers," said Joshua N. Leonard, the senior author of the study. "The simple cell rewiring we've done ultimately could help overcome immunosuppression at the tumour site, one of the most intransigent barriers to making progress in this field."
When cancer is present, molecules secreted at tumour sites render many immune cells inactive.
The Northwestern researchers genetically engineered human immune cells to sense the tumour-derived molecules in the immediate environment and to respond by becoming more active, not less.
This customised function, which is not observed in nature, is clinically attractive and relevant to cancer immunotherapy.
The general approach for rewiring cellular input and output functions should be useful in fighting other diseases, not just cancer.
"This work is motivated by clinical observations, in which we may know why something goes wrong in the body, and how this may be corrected, but we lack the tools to translate those insights into a therapy," Leonard said. "With the technology we have developed, we can first imagine a cell function we wish existed, and then our approach enables us to build -- by design -- a cell that carries out that function."
Currently, scientists and engineers lack the ability to program cells to exhibit all the functions that, from a clinical standpoint, physicians might wish them to exhibit, such as becoming active only when next to a tumour.
This study addresses that gap, Leonard said.
Leonard, who focuses on integrating synthetic biology into medicine, is an associate professor of chemical and biological engineering at the McCormick School of Engineering.
He is a member of the Robert H. Lurie Comprehensive Cancer Center of Northwestern University.
The research comes out of a rich collaboration that Leonard's team has with clinical oncologists, immunologists and basic cancer researchers at Northwestern University Feinberg School of Medicine as well as other synthetic biologists.
The study, published by the journal Nature Chemical Biology, provides details of the first synthetic biology technology enabling researchers to rewire how mammalian cells sense and respond to a broad class of physiologically relevant cues.
Kelly A. Schwarz, a graduate student in Leonard's research group, is the study's first author.
"This work is exciting because it addresses a key technical gap in the field," Schwarz said. "There is great promise for using engineered cells as programmable therapies, and it is going to take technologies such as this to truly realise that goal."
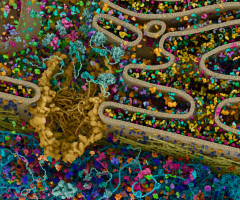
Starting with human T cells in culture, the research team genetically engineered changes in the cells' input and output, including adding a sensing mode, and built a cell that is relevant to cancer immunotherapy.
Specifically, the engineered cells sense vascular endothelial growth factor (VEGF), a protein found in tumors that directly manipulates and in some ways suppresses the immune response.
When the rewired cells sense VEGF in their environment, these cells, instead of being suppressed, respond by secreting interleukin 2 (IL-2), a protein that stimulates nearby immune cells to become activated specifically at that site.
Normal unmodified T cells do not produce IL-2 when exposed to VEGF, so the engineered behaviour is both useful and novel.
This work was carried out in cells in culture, and the technology next will be tested in animal studies.
While Leonard's team has initially focused on the application of this cell programming technology to enabling cancer immunotherapy, it can be readily extended to distinct cellular engineering goals and therapeutic applications.
Leonard's "parts" are also intentionally modular, such that they can be combined with other synthetic biology innovations to write more sophisticated cellular programs.
"To truly accelerate the rate at which we can translate scientific insights into treatments, we need technologies that let us rapidly try out new ideas, in this case by building living cells that manifest a desired biological function," said Leonard, who also is a founding member of the Center for Synthetic Biology and a member of the Chemistry of Life Processes Institute.
"Our technology also provides a powerful new tool for fundamental research, enabling biologists to test otherwise untestable theories about how cells coordinate their functions in complex, multicellular organisms," he said.
Source: Nature Chemical Biology
The World Cancer Declaration recognises that to make major reductions in premature deaths, innovative education and training opportunities for healthcare workers in all disciplines of cancer control need to improve significantly.
ecancer plays a critical part in improving access to education for medical professionals.
Every day we help doctors, nurses, patients and their advocates to further their knowledge and improve the quality of care. Please make a donation to support our ongoing work.
Thank you for your support.