A phase 1b study of vadastuximab talirine in combination with 7 3 induction therapy for patients with newly diagnosed acute myeloid leukemia (AML) has been presented at ASH 2016.
In a clinical trial, vadastuximab talirine (33A) was found to be safe when used in combination with standard chemotherapy treatment for patients with AML.
The trial results raise researchers’ hopes that this investigational, targeted therapy can help patients achieve more complete cancer remission and reduce the likelihood of relapse.
33A is being developed as a complement to standard chemotherapy in an effort to reduce the need for multiple rounds of chemotherapy to induce initial remission and to improve long-term outcomes.
The standard treatment for AML, which consists of a continuous infusion of cytarabine for seven days plus infusion of an anthracycline for three days (often called 7 3), has been in use for decades but achieves an overall cure rate of just 40–50 percent in patients younger than 60 years.
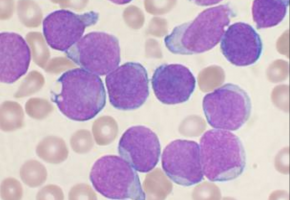
33A is designed to seek out CD33, a protein found on leukaemic blasts in roughly 90 percent of AML patients, and kill these targeted cells.
This Phase 1b study included 42 patients who were administered 33A along with standard chemotherapy.
Patients showed no evidence of increased toxicity or mortality, and the rates of adverse effects were similar to what would be expected with standard chemotherapy alone, according to the researchers.
No patients experienced infusionrelated reactions, venoocclusive disease, or significant liver damage.
The most commonly reported side effects were nausea (reported by 55% of patients), diarrhoea (33%), and constipation (31%).
Researchers said the outcomes were also encouraging from an efficacy standpoint because a higher-than-expected portion of patients achieved remission after a single round of treatment.
A total of 78 percent of patients achieved remission, with 60 percent achieving complete remission (CR) and 18 percent achieving remission with incomplete blood count recovery (CRi).
In addition, highly sensitive tests showed many patients had no evidence of the disease 28 days after starting treatment, suggesting the drug may lead to a more complete remission than standard chemotherapy alone.
“I think we can safely give vadastuximab talirine in combination with chemotherapy,” said lead study author Harry Erba, MD, PhD, of the University of Alabama at Birmingham. “The next question to study is whether it improves long-term disease-free survival. There’s much reason to be hopeful that such an investigation will have positive results.”
Source: ASH 2016
The World Cancer Declaration recognises that to make major reductions in premature deaths, innovative education and training opportunities for healthcare workers in all disciplines of cancer control need to improve significantly.
ecancer plays a critical part in improving access to education for medical professionals.
Every day we help doctors, nurses, patients and their advocates to further their knowledge and improve the quality of care. Please make a donation to support our ongoing work.
Thank you for your support.