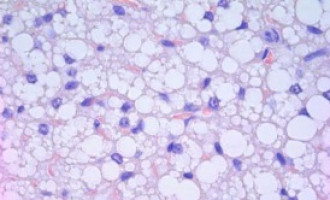
New research has found a subset of our immune cells (called regulatory T cells) that are highly abundant in the tumour microenvironment and are particularly good at suppressing the anticancer immune response.
In two independent studies, published November 15 in Immunity, scientists describe the distinct features and differences in molecules expressed by regulatory T cells inside of human breast, colon, and lung tumours compared to normal tissue that could be potential biomarkers or therapeutic targets.
Both sets of researchers hope to use what they've learned about the unique properties of regulatory T cells in tumour sites to improve cancer immunotherapies—drugs that stimulate immune cells to attack cancer cells.
While these treatments have been successful for some types of tumours, such as melanoma, up to 40% of patients report serious adverse events.
"Our working hypothesis is that most of the adverse effects that patients experience with these immunotherapy treatments is because they are targeting molecules that are present both on regulatory T cells in the tumour and regulatory T cells outside of the tumour," says Sergio Abrignani, co-lead author on one of the studies with Massimiliano Pagani, both of the Istituto Nazionale Genetica Molecolare "Romeo ed Enrica Invernizzi" and Università degli Studi di Milano in Italy.
"If we target molecules that are selectively present in the tumours, then we would have comparable efficacy and fewer adverse events," adds Pagani.
"We are discovering a lot of new markers for these cells that can be used to make future therapies safer."
Their study, part of the International Human Epigenetics Consortium, specifically analysed tissue samples collected from nearly 200 patients with colon and lung cancer and compared them to normal tissue and peripheral blood.
The researchers identified specific signature molecules and genes not previously associated with regulatory T cells that could be detected in both primary and metastatic tumours.
Certain molecules may even be potential biomarkers for poor prognosis.
"We know that tumours that are highly infiltrated with regulatory T cells are bad, but our paper also shows that tumours with the highest expression of signature molecules on intratumoral regulatory T cells had the worst outcomes," Abrignani says, noting that clinical trials on new biomarkers and immunotherapies inspired by this study could begin in as soon as two years.
"We've set the stage for a bunch of important studies that must be done as soon as possible."
The other Immunity study, led by Alexander Rudensky of the Ludwig Center at Memorial Sloan Kettering Cancer Center, looked specifically at the distinct feature of regulatory T cells from over 100 human breast tumours removed during surgery.
His group found that compared to normal tissue and peripheral blood, breast tumours possess an increased presence of regulatory T cells and that the most aggressive breast cancers have the highest number of the cells.
In the analysis of the immune cells by Rudensky's team, the most notable contrast was increased expression of chemokine receptor protein CCR8 in the tumour-resident cells in breast and other cancers (also found to be overexpressed in colon and lung tumours in Abrignani and Pagani's study).
Why CCR8 may be significant is still unknown, but it offers itself as another potential target for immunotherapy.
"What's remarkable is the differential expression of CCR8; it is a very clear and clean marker that distinguishes regulatory T cells in the tumour," says Rudensky, also of the Howard Hughes Medical Institute.
"This suggests one path to a more selective strategy to deplete regulatory T cells present in breast and other types of cancer."
Many questions still remain about the relationship between regulatory T cells and cancer, as well as why some of their unique properties promote immunosuppression.
It will be helpful to learn, for example, why more aggressive tumours have an increased number of regulatory T cells—are they better at recruiting the cells or are there more at the tumour to begin with—as well as what triggers from the tumours are changing the regulatory T cells' behaviour.
"It is a really exciting time for both basic researchers and cancer biologists as we reveal a more complete picture of the interactions between different immune cell types and the tumour microenvironment," Rudensky says.
Reference
De Simone, Arrigoni, Rossetti, and Gruarin et al. Transcriptional landscape of human tissue lymphocytes unveils uniqueness of tumour T regulatory cells, Immunity, November 15, 2016
Plitas and Konopacki et al. Regulatory T cells exhibit distinct features in human breast cancer, Immunity, November 15, 2016
Source: Cell Press