Although many cancer patients respond favourably to immunotherapies such as nivolumab and pembrolizumab, most patients do not.
Blame for treatment failures is usually attributed to so-called "cold" tumours, those that do not attract T-cell infiltration and may lack key T-cell targets--the mutated proteins known as neoantigens.
Teams from the University of Chicago and Johns Hopkins University have published a pair of related studies looking at biomarkers involved in the immune system's response to tumours in the Proceedings of the National Academy of Sciences.
The University of Chicago study, looking at 266 metastatic melanomas, found no difference in the number or types of neoantigens found in "hot" T-cell-inflamed and "cold" non-T-cell-inflamed tumours.
The study provides evidence that the lack of T-cell activation and infiltration in non-T-cell-inflamed tumours was more likely caused by the inability to recruit and activate a specific group of dendritic cells, which process antigens and present them to T cells.
Instead of the presence of fewer antigens, "we found that these tumours are full of antigens but lack evidence for a subset of dendritic cells, known as Batf3 DCs," said Thomas Gajewski, MD, PhD, professor of pathology and medicine at the University of Chicago and senior author of the study.
"Those cells initiate immune reactions," he said. "Understanding this process gets us closer to treatments that will expand the percentage the patients who respond to anti-PD-1 drugs and other immunotherapies."
"This model," the authors wrote, "accounts for more of the available data than does the hypothesis that this subset of tumours lacks antigens for recognition."
The results come as a relief for those in the field, explained Stefani Spranger, PhD, senior post-doctoral fellow at the University of Chicago and the study's co-lead author.
"There was widespread concern that activating T cells might require some baseline level of mutational burden in the tumour environment," she said. "If inflammation and the presence of mutations were tightly linked, then the mutations that could trigger an immune response might not be present in un-inflamed tumours. So, even if we lured T cells in, they might not see any good targets."
"Fortunately, this was not the case," she added. "We found abundant good antigens, as many in non-inflamed as in T-cell-inflamed tumours. Now we have to devise better ways to get the T cells over the wall and into non-inflamed tumours."
"This research lays a framework for understanding the spectrum of T cell inflammation across tumour types and emphases that mutational density and neo-antigen load are not the only factor driving responsiveness to checkpoint immunotherapy," added co-first author Jason Luke, MD, assistant professor of medicine at the University of Chicago. "As biomarkers of responsiveness develop, we will need to analyse multiple forms of data in individual patients to maximize treatment outcomes."
There are tools to do this, suggests Gajewski.
"We are looking at ways to manipulate various pathways, such as using STING agonists or Wnt/Beta-catenin pathway blockers, which can limit T-cell infiltration of the tumour environment." Locally manipulating the signalling systems that restrict T cell access could be therapeutic.
The National Cancer Institute and Bristol Meyers Squibb funded this research.
Additional authors include Riyue Bao, Yuanyuan Zha, Kyle Hernandez, Yan Li, Alexander Gajewski and Jorge Andrade.
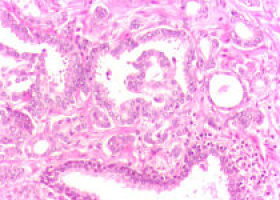
The Johns Hopkins scientists studied 3,500 tumour samples among nine cancer types recorded in The Cancer Genome Atlas to analyse five biomarkers of immune activity within tumours.
They include: whether the microenvironment within a tumour is inflamed, the number of mutations present in tumour cells, and expression levels of immune-system related proteins called PD-1, PD-L1, and PD-L2, which can be coordinately expressed in the environment surrounding a tumour to ward off an immune system attack.
"Scientists have been looking at these markers independently, but we wanted to know how they relate to each other and which was most influential in patients' survival," said Janis Taube, MD, associate professor of dermatology and pathology at the Johns Hopkins University School of Medicine and member of the Johns Hopkins Kimmel Cancer Center and its Bloomberg-Kimmel Institute for Cancer Immunotherapy.
Taube and her team found that all five factors were important in predicting survival of patients with metastatic melanoma.
Four of the factors -- PD-1, PD-L1, PD-L2 and inflammation -- have very tight links, they say, and their research suggests that when expression levels of these factors are high, they are more important in predicting patients' survival than the amount of mutations present in the tumour.
However, when these factors are low, mutational load plays an important role in predicting survival.
"This is an important step in understanding how to develop multifactorial-biomarkers for predicting patient outcomes," Taube said.
Source: PNAS